Chapter 25: Mental health risk assessment: a personalised approach
Case Study: High risk indicators
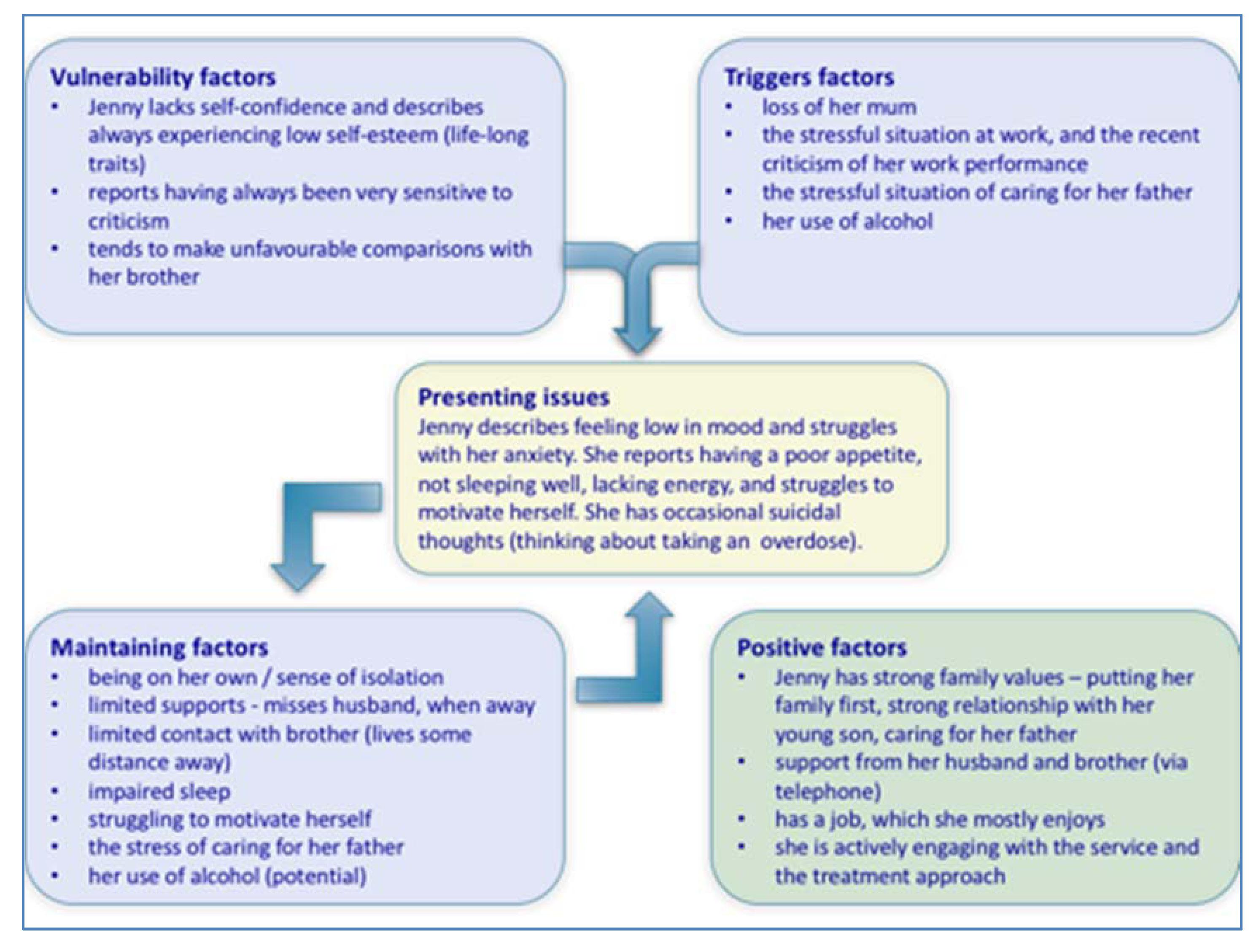
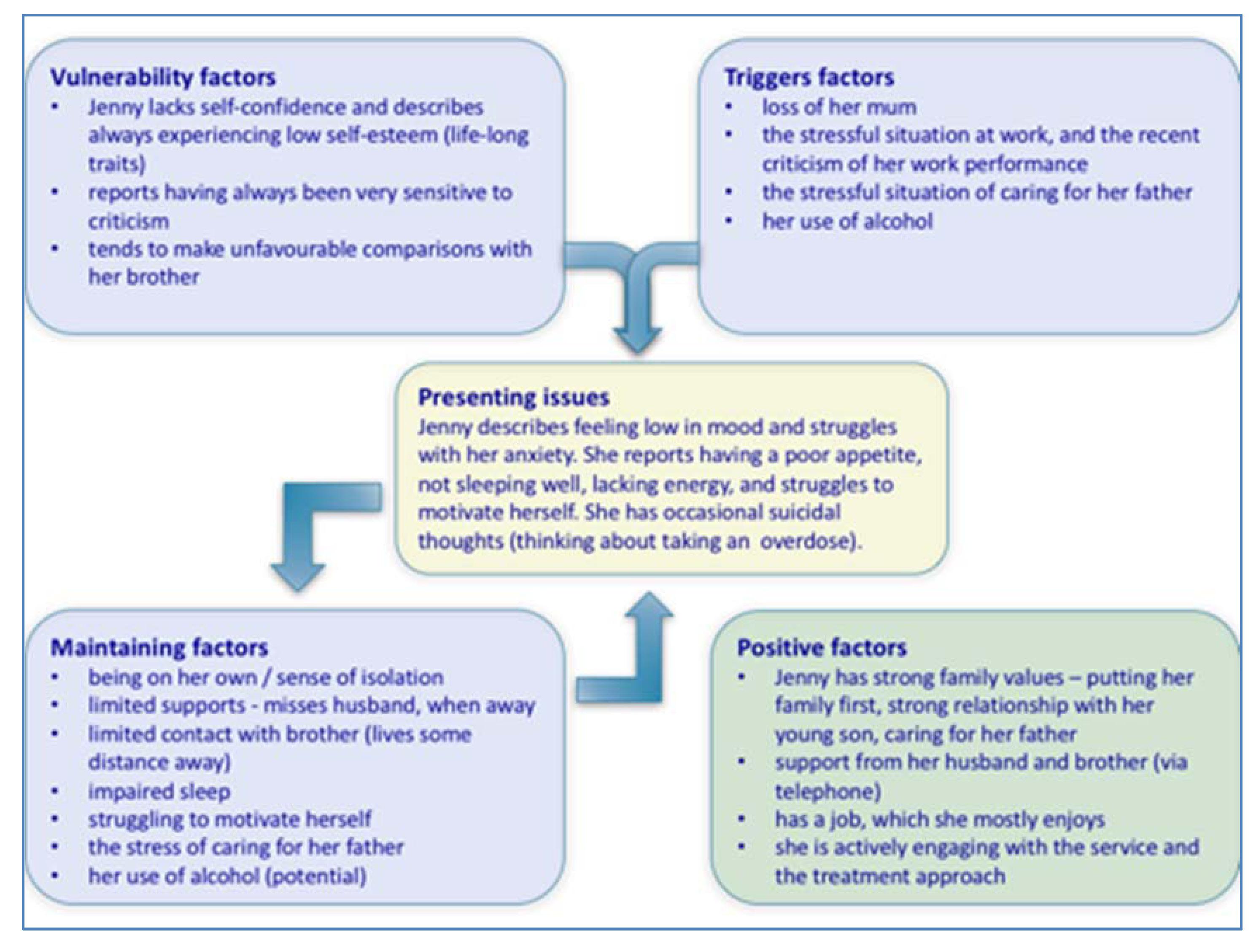
Jenny is 35 and lives with her husband and 9-year-old son. Though employed as a welfare officer, she has felt unable to work for over three months. A new manager joined her team six months ago, and has criticised her work performance on several occasions. Jenny has felt low since her mother died a year ago, to whom she was very close. She has been finding it difficult to motivate herself, is struggling to sleep properly, has begun to think that everything is pointless and is going wrong, and has again begun to think about taking an overdose. She believes that her husband has had enough of her ‘moods’ and irritability, and fears he may leave her.
Jenny has had two in-patient admissions in the last four years, each precipitated by her taking a significant overdose of prescribed antidepressant and anxiolytic medication, with alcohol. On each occasion, she had felt highly stressed for a prolonged period: moving accommodation; trying to complete a college course; trying to look after her young son; missing her husband whilst he is away working as a lorry driver.
Jenny has again been feeling very stressed, particularly when trying to respond to the demands of her 77-year-old, proud and independent father, who lives nearby – becoming increasingly infirm, he has had a couple of recent falls. Jenny has always had a difficult relationship with her father, who is often critical of her and always favoured her brother. Though close to her only brother, he lives over 200 miles away.
- What are some relevant examples of static and dynamic risk factors?
- Which would merit special attention as ‘high’ risk indicators?
- What are some relevant protective factors?
- Which structured assessment tools might be helpful in complementing the assessment process?
- What might be some limitations of these tools?
- Sketch out a formulation using the 5Ps framework.
- What ideas would this give you about the specific focus for treatment and care?
› Possible answer
- What are some relevant examples of static and dynamic risk factors?
- e.g. sensitive to criticism, history of overdoses, loss (of mother), prolonged stress, limited supports, sense of isolation, hopelessness, suicidal ideation.
- Which would merit special attention as ‘high’ risk indicators?
- e.g. previous significant risk behaviour, prolonged stress (given her previous experiences), active suicidal intent (planning and preparation).
- What are some relevant protective factors?
- e.g. strong family values/relationships, support from husband and brother, having a job, positive and active engagement with the mental health service, previous response to treatment and recovery.
- Which structured assessment tools might be helpful in complementing the assessment process?
- e.g. START, Beck Hopelessness Scale, Beck Suicide Intent Scale, a Depression Inventory, mood diary/thought record, baseline activity monitoring schedule, sleep chart, and a simple mood scaling record.
- What might be some limitations of these tools?
- e.g. level of subjectivity, potential bias in completion (both for self and observer/practitioner rated tools), over-focus upon symptoms, potential for increasing distress, poor use/completion as a consequence of features of the illness (e.g. low motivation).
- Sketch out a formulation using the 5Ps framework.
- Compare your sketch with the following example formulation diagram
7. What ideas would this give you about the specific focus for treatment and care?
Compare your response with the following – you may have considered assisting Jenny to:
- form an illness timeline.
- set and work towards personal goals – incorporating opportunities for positive risk taking.
- form a rationale and engage in the following interventions – as examples:
- sleep promoting strategies.
- building confidence and cultivating self-esteem.
- activity planning and self-monitoring.
- developing skills in structured problem-solving.
- recognising and responding to unhelpful thoughts.
- practising methods of relaxation and stress management.
- mobilising her support network .
- staying well planning (relapse prevention planning).
- pharmacological option (as part of a combined pharmacological and psychosocial approach): anti-depressant medication.