Health Promotion: Planning & Strategies
Namibia
Health extension programme increasing access and utilization of health services in Namibia
Pandu Hailonga-van Dijk
Seahorse Research and Training Institute
Desderius Haufiku
Department of Health Policy and Management, School of Public Health, University of Namibia
Keywords: Health extension workers, community health workers, community volunteers, empowerment, public health policy, training
Summary
The Ministry of Health, faced with limited human health resources and inspired by the Alma Ata Declaration commitment, initiated the health extension programme. Aware of the contribution community volunteers made on HIV/AIDS prevention and management, over 1500 community health workers have been employed across 12 regions since 2012. Their primary role is to increase access to health services, through education, campaign, empowering community members by creating awareness of health determinants, disease prevention and managing health and ill health. Health extension workers (HEWs) consider the role of the multiple levels influencing health, focusing on individual empowerment, community participation and equity.
Setting and context
Namibia has a population of 2.3 million and is a sparsely populated country, with an estimated 2.6 persons per sq km, making access and utilization of health services a challenge. The DHS reported 31% of the population found distances from health facility a barrier to accessing health.
Challenging terrains between remote communities and health facilities remain a major challenge. Penchansky and Thomas (1981) identified five key elements playing a critical role in health provision, accessibility; availability; affordability; acceptability and accommodation. Although government subsidies give free health services to community members, the 2014 National Quality Assessment found 48% of patients travelled more than 5 km to a health facility
Pre-independence, Namibia health care was racially based, urban centric, fragmented. Post-independence health care gave Primary Health Care a community based preventative focus.
Human resource for health is a major challenge, as a result in 2012, the Ministry of Health and Social Services (MOHSS) trained the first 34 HEWs in the Kunene region to address disease prevention, promote health and access community health. Around 1,600 HEWs are in 12 regions.
Aims and objectives
Raising awareness through community education campaigns is HEWP’s primary purpose. In the process, empower community members to manage their health determinants, disease prevention and minor ailments. Figure 1 provides an overview of the HEW areas.
The key objectives are as follows
- Increase access to, and coverage of, promotive, preventative, rehabilitative and basic curative services with focus on maternal, neonatal and child health and nutrition
- Strengthen and expand the continuum and quality of care and support, including bi-directional referral between the community and the health facility
- Empower local communities through awareness building and training of Community Based organizations to promote healthy lifestyles
- Promote ownership and participation through the involvement of community members in planning, implementation and monitoring of HEP
- Collect and analyse household level data for planning, reporting and decision making
|
Hygiene and environmental sanitation |
Disease prevention and control |
Family health services |
Health education and communication |
|
Proper and safe excreta disposal system |
Prevention and control of HIV/AIDS |
Maternal and child health |
Health education and communication |
|
Proper and safe solid and liquid waste management |
Prevention and control of tuberculosis |
Family planning |
Water supply safety measures |
|
Healthy home environment |
Prevention and control of malaria |
Immunization |
Food hygiene and safety measures |
|
Personal hygiene |
First aid |
Adolescent reproductive health |
|
|
|
|
Nutrition |
|
Figure 1: Major areas and packages of HEWs
Description of main features
CHWs are frontline public health workers who are trusted members of and/or have an unusually close understanding of the community served. This trusting relationship enables CHWs to serve as a liaison/link/intermediary between health/social services and the community to facilitate access to services and improve the quality and cultural competence of service delivery. CHWs also build individual and community capacity by increasing health knowledge and self-sufficiency through a range of activities such as outreach, community education, informal counselling, social support and advocacy (APHA, 2009).
Phase 1: Facing the imminent challenge of communicable diseases
At independence, Namibia depicted health inequality with most of communities having no access to health and social services. While the health systems post-independence was being restructured, there was a HIV/AIDS epidemic, further complicated by the lack of health professionals and overstretched health facilities. This made community volunteers an important resource, not only to care for the sick, but also to educate communities on disease prevention.
CHWs re-emerged in the late 90s as a valuable resource, the response backbone, even though they were mainly volunteers, they greatly reduced the HIV/AIDS burden on the health system. The programme, largely dependent on donor funding, had challenges with coordination, supervision and sustainability (PMU, 2014).
Global studies found CHWs played a critical role in achieving the Millennium Development goals. It is anticipated that they will play an important role in achieving the Sustainable Development Goals (SDGs).
Phase 2: Policy debate and pilot
In 2008, the Namibia health system review, identified a gap between the health facility and the community, recommended extending health services to communities through the establishment of health extension programmes (HEP). The National Health Strategic Plan identified HEP among key strategies giving Namibians access to health services as reflected in the 2013 cabinet decision. The process ensured that the programme fitted national priorities and located within the Primary Health Care department.
The government created an enabling environment, CHWs were integrated into the health workforce; with finances for salaries, training, equipment and supplies made available. International organizations provided technical and financial support. Community members were actively consulted. They collaborated on matters such as who to recruit, the role and which communities to serve.
Phase 3: The first pilot in Kunene
The first pilot project was introduced in Kunene in 2012. UNICEF and USAID/C-CHANGE collaborated with the Namibia Government to provide both financial and technical assistance. Support included guidance, payment of allowances in Kunene, development, training materials reviewing, roll out training, supervision, meetings, master plan development, as well as procurement of supplies and equipment.
The programme started with 34 trainees selected from the identified communities, which had some of the worst health indicators. After six months training, they worked in their respective communities providing for first aid, maternal, post-natal care, child health and nutrition, HIV/AIDS, Malaria and TB. They became the link between communities and the health facilities.
The pilot was successful and preliminary findings noted improvements in health-related behaviour. The programme received the blessing of the management, community members and government. There are four key factors that contributed to the success of the pilot i.e. i) Political commitment and leadership; ii) integration of CHW into the Health sector; iii) Community ownership and iv) Buy in and involvement of key stakeholders.
Phase 4: Expansion to implement country wide
Following pilot project, the Government expanded the programme which include a strong monitoring system. Currently, there are 1640 CHWs serving 12 regions out of 13.
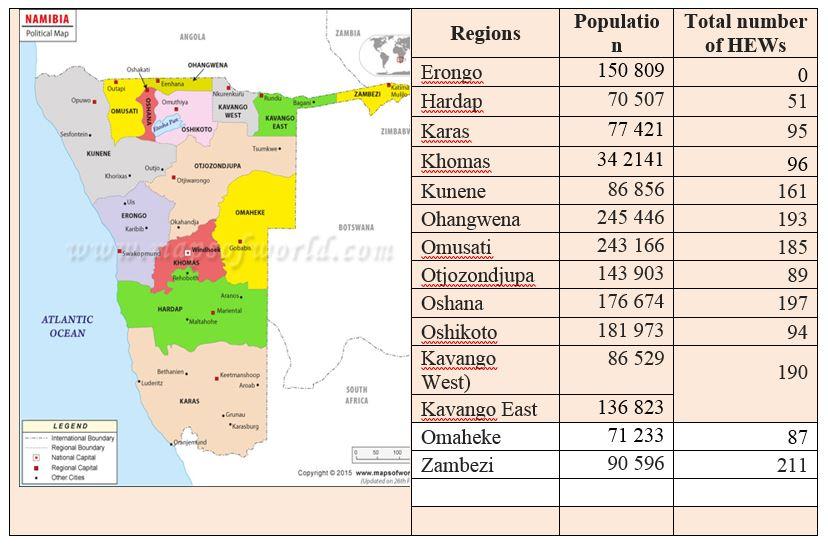
Figure 2: Deployment of HEWs in Namibia
Application to key principles of health promotion and relevant theory
The Namibian HEW programme employs several frameworks: (i) community empowerment model, (ii) socio ecological framework and (iii) adult learning theory.
The HEW’s programme combines/involved individuals, community members, leaders, social networks and mass communications. It has given the rural poor, who have been historically excluded because of structural, social, economic and cultural factors, who are facing geographic challenges, culturally inappropriate services combined with poor health literacy and language barriers, a voice.
The programme acknowledges that the most effective way to address health-related challenges is through community empowerment, whereby communities are informed and educated to gain insight into their own situation and to identify collectively, solutions for the betterment of their health. Community ownership is one key ingredient in the successful implementation of the HEP. Figure 3 provides an overview of the community empowerment model.
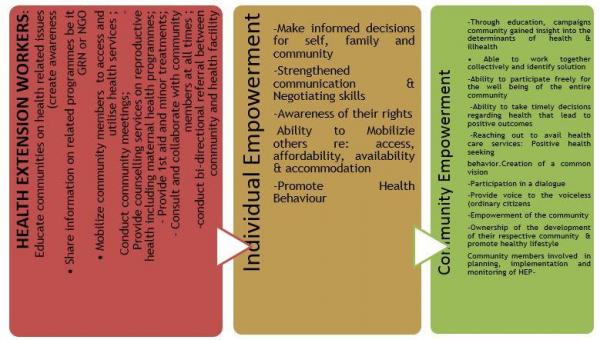
Figure 3: Overview of the community empowerment model
Whiteheads’ socio-ecological framework provides an overall view of social determinants for health. HEP acknowledges that health is the result of multiple factors at multiple levels from the individual life style, social and community networks, living and working condition, socio economic cultural and environmental conditions and places it in the broader government principles. Figure 4 provides an overview.
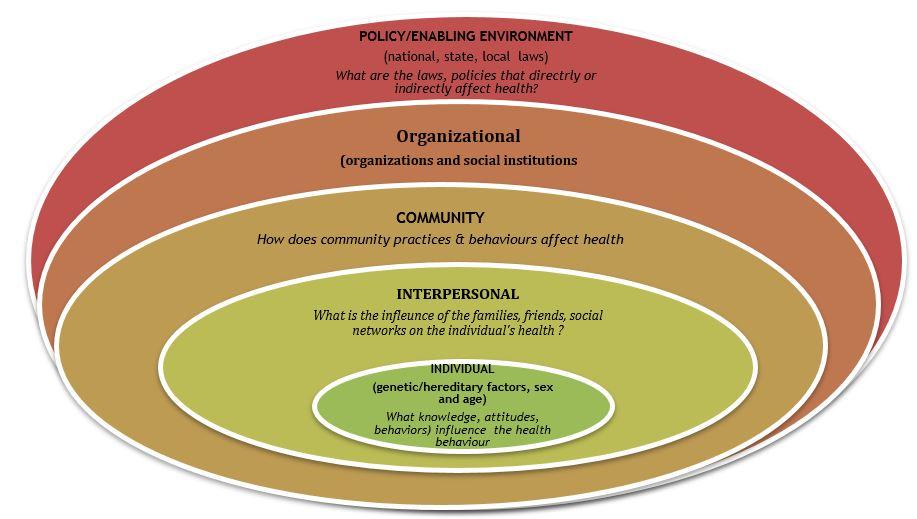
Figure 4: Socio-ecological framework
The programme acknowledges that for the HEWs to conduct quality work, they should be trained in adult learning and facilitation skills, as their learning influence how they will educate communities and individual. Hence, they are strengthened to impart knowledge in an empathetically manner and in a language, that is understood by the individual and communities. Similarly, in Brazil the CHWs draw from Freire’s philosophy of learning and teaching which emphasizes the value of indigenous knowledge (Pinto, da Silva, & Soriano, 2012).
Useful Link
References
-
APHA. (2009). Support for community health workers to increase health access and to reduce health inequities. Policy number: 20091 Retrieved from: www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2014/07/09/14/19/support-for-community-health-workers-to-increase-health-access-and-to-reduce-health-inequities
-
The Namibia demographic and health survey 2013. Windhoek, Namibia, and Rockville, Maryland: MoHSS and ICF International.
-
Penchansky, R., & Thomas, J. W. (1981). The concept of access: Definition and relationship to consumer satisfaction. Medical Care, 19(2), 127–140.
-
Pinto, R. M., da Silva, S. B., & Soriano, R. (2012). Community health workers in Brazil’s unified health system: A framework of their praxis and contributions to patient health behaviors. Social Science & Medicine, 74(6), 940–947. doi:10.1016/j.socscimed.2011.12.025.
