Introduction to Human Resource Management
Author Case Studies
Workforce Planning in Practice at NHS London
In September 2008, NHS London published Workforce for London: A Strategic Framework, outlining the way in which the organisation was to address a number of key challenges facing health care in the capital over the coming decade. These include a rapidly growing population (predicted to equate to 600,000 additional users of health services over the next ten years) and the highly variable quality of health care provision, resulting in the highest rates of ‘consumer’ dissatisfaction in England. These challenges, along with a stated strategic objective to provide world-class health care for every Londoner, have significant implications for the size, shape and distribution of London’s health care workforce.
The current workforce
London’s complex health care system has the highest number of constituent NHS organisations in the UK and employs over 205,000 staff, 15.4 per cent of the total NHS workforce. It has some of the world’s leading medical centres of excellence which form a national and international hub for innovation in clinical care, research and education. However, the report also outlines a number of key staffing issues faced by NHS London, including:
- In London hospitals, the ratio of clinical staff to occupied beds varies from 0.9 to over 2.0.
- The lowest staffing levels are often in the areas with the greatest need – more GPs are in the south and west of London than in the more deprived east and north.
- London has more doctors (30.8 doctors per 10,000 population compared to an England average of 21.2) but fewer nurses (62.5 nurses per 10,000 population against an England average of 67.5) when compared with the rest of England.
- As a result of historic recruitment patterns and more staff delaying retirement, there is now a higher proportion of older staff in the workforce than ever before.
Health care has always attracted a large proportion of female workers, and there continue to be growing numbers of women in the medical workforce. It is anticipated that working hours per week in the medical workforce will reduce over the next ten years, reflecting a greater demand for flexible working arrangements by both men and women and the need for compliance with the European Working Time Directive by 2009, which imposes a maximum of 48 working hours per week. Advances in technology will also have a significant impact on the shape of London’s workforce through the creation of more centres with the technology and expertise to deliver highly specialised, complex care, and through the development of assisted technology, enabling care to be delivered closer to home. This will require the redesign of working patterns, the development of new skills and expertise and the opportunity to create new roles. London plays an important role both nationally and internationally in training and developing future health care professionals but suffers from high labour turnover and loss of key staff to other parts of the country. For example, London trains 29 per cent of UK medical undergraduates but over a third of these students do not work there after graduation. For nursing and midwifery, London’s share of students (18.3%) is in proportion to the number of staff employed (17.7%). However, it is believed that London exports qualified and experienced staff to the rest of England, as demonstrated by consistently higher vacancy rates.
Workforce for London: a strategic framework
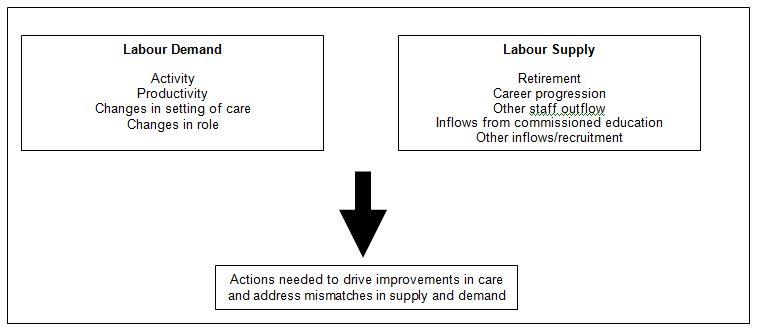
The purpose of the review which led to the strategic framework was to assess the impact of anticipated changes in health care needs, demographic trends, technology and patient and public expectations on the future size, shape and composition of London’s health care workforce and the changes required to how the organisation plans, trains, develops and deploys its employees. To assist in the workforce planning process, NHS London employed scenario modelling to provide insight into the strategic challenges ahead, and how these will affect the overall shape and size of London’s workforce.
Scenario modelling approach taken in Workforce for London
The resulting strategic framework identified a number of both quantitative and qualitative changes in the NHS workforce needed to meet the challenges of the coming decade. In broad terms, the strategic framework acknowledged the central role played by the workforce in high quality service delivery but identified that staff were not fully utilised (productivity levels of staff in London were lower than elsewhere in England). The review suggested that London’s NHS workforce will need to grow by between 4 and 23 per cent over the next ten years, dependent on the level of productivity delivered. The framework outlined three broad strands in how NHS London should respond to the demand and supply forecasting process.
The first focuses on the quantitative dimensions of the required workforce needed to increase productivity, to improve service quality and to address wider initiatives in the NHS regarding the delivery of care. The review indicated a need to develop new roles and new skills through increased targeted workforce development and investment. For example, the review advocates the development of broader sets of skills across the workforce. The review also suggests changes to where and how practitioners work, particularly through providing care closer to people’s homes. The review also suggests enhancing employment opportunities for Londoners to reduce turnover, and to develop a workforce more representative of the community it serves.
The second element focuses on the systems required to support this ‘new’ workforce. In particular, it stresses the importance of the effective integration of workforce planning, and educational investment, with service needs, particularly through the localisation (as far as possible) of workforce planning, tailored to meet the diverse needs of patients.
Finally, the framework proposes a number of changes to leadership processes, with a particular focus on fostering a climate of worker engagement and empowering frontline staff to ‘improve and develop the services they provide, creating new freedoms to innovate and provide the leadership for local change’. In response to recent staff surveys, NHS staff indicated that a positive relationship with staff tends to relate to improved performance and the framework indicates a desire to engender teamworking and ‘partnership’ across the organisation. The framework also indicates a need to develop excellent leaders at all levels of the organisation and to develop a pipeline of talent for chief executive and director roles across the capital.
Questions
- What are the pertinent factors that are shaping the supply and demand for medical practitioners in London over the coming decade? To what extent are these factors reasonably predictable?
- What responses to the workforce planning process are outlined in the case study?
- Why might the formal approach to workforce planning used by NHS London not necessarily be appropriate in many private sector organisations?
- How can HR planning contribute to the achievement of organisational objectives in all organisations?
