Essentials of Nursing Children and Young People
Student Resources
Anatomy and Physiology Links
Chapter 17: Caring for children and young people in the peri- and postoperative recovery period
17.1 Thermoregulatory needs
With reference to A&P the differences between thermoregulatory needs of all age children and young people can be explored/identified, meaning different aged children will require different nursing care.
Three heat processing steps must be understood in order to understand temperature control:
- Heat Generation – the process by which heat is produced (generally in the body core)
- Heat Conservation (Insulation) – the mechanisms by which heat is restricted from reaching the body surface (generally done at the periphery)
- Heat Loss – physical processes of heat loss from the body surface
Heat generation can occur through: basal metabolism resulting in heat – the heat generated by this mechanism is proportional to mass; shivering; and the use of large body movements. Newborn babies also have brown fat that can be metabolised to generate heat. Heat production from brown fat relies on central nervous system arousal leading to metabolism of brown fat. This brown fat is specific to this age group and therefore older children do not have this method of heat generation.
Heat conservation depends on insulation (white fat lining dermis). Neurological control of the blood vessels connecting the superficial and deep venous plexuses (on opposite sides of the fat) in the skin determine how much blood reaches the cool areas peripheral to the white fat. In order to raise body temperature these vessels are closed and blood does not reach the periphery (the body appears mottled, blue and feels cold). In order to lower the body temperature, these vessels are opened and blood reaches the skin surface (the body is flushed, red and feels warm).
Heat loss can occur through evaporation (liquid to gas transfer of heat, e.g. sweating), conduction (solid to solid contact, e.g. sitting on cold surfaces), radiation (solid to solid at a distance transfer of heat, e.g. sitting near cold objects) and convection (solid to gas transfer of heat, e.g. cold breeze/draughts).
To maintain a constant body temperature, heat production must equal heat loss from the body surface over a given time. Heat production in infants is low relative to heat loss. Infants are at highest risk of developing hypothermia due to their heat loss from conduction (infants tend to have larger percentages of their total body surface area in contact with the mattress) and convection (large body surface area to weight ratio). They are also less able to respond to cold stress due to radiation (less able to move from cold objects) and evaporation (if wet, rely on others to remove wet items). They will therefore need to have thermoregulatory needs provided for them. Infants may require incubators and additional clothing (e.g. hats) or blankets to maintain heat, especially when being transferred from the ward to the theatre for surgery.
The larger child/young person will be able to generate more heat from shivering, generating large body movements and through basal metabolism (heat production is proportional to mass). In addition, they are more likely to have better neurological control over heat conservation methods. Finally, depending upon the age of CYP, they may also be able to manage heat loss mechanisms. However, if a CYP is unwell, then they may be less able to respond to the heat loss or gain and so the CYP nurse must be mindful of this, especially during transfer to theatre, when corridors may be draughty and colder than the ward area.
17.2 Skin & wound healing
Stage 1: Haemostasis
This is a newly sustained wound which may be bleeding and painful for the patient.
When the skin integrity is breached, bleeding occurs and platelets aggregate (clump together) to form a clot over the damaged area of the blood vessel. Clots mainly consist of fibrin, which creates a scaffold to support new migrating cells (see Stage 2).
Stage 2: Inflammation
This stage can start as soon as the wound is sustained and can last up to five days.
The clot begins to break down and the surrounding capillaries dilate, making them more permeable, which causes fluid to leak into the wound site. White cells (neutrophils, macrophages and lymphocytes) are activated. Neutrophils ‘wash’ through the site for up to three days in order to destroy bacteria (by phagocytosis), then reduce in number unless there is infection. Macrophages also destroy bacteria and initiate the next stage of healing.
As part of the inflammatory process, mast cells release histamine and other substances.
The wound bed may have:
- yellow, cream or brown tissue called slough, which consists of old fibrin and destroyed bacteria.
- dead tissue called necrotic tissue, which can appear dark brown or black and may be moist or hard and leathery.
Dilated capillaries will mean the area surrounding the wound will be red or flushed (inflamed) and fluid leaking from the capillaries will cause swelling around the wound (oedema). This oedema will increase pressure in the tissues and may be painful.
Stage 3: Proliferation
This may last for days or weeks depending on the extent of the injury. The space that has resulted from the wound fills up with granulation tissue, a structure composed of various cells including fibrin, keratin, collagen and glycoproteins.
The swelling will be subsiding and the wound will be filling with red, moist, shiny granulation tissue. There will be evidence of new tissue at the wound edges (epithelialization). The epithelialization will appear paler than the original skin because it is new.
Macrophages in the previous stage have stimulated the production of fibroblasts, which now enable the growth of new blood vessels. Elastin is also produced, which gives the new tissue resilience and elasticity.
Once the wound is filled with new granulation tissue, a process of re-epithelialization occurs, starting at the wound edges and from any epithelial cells in the wound bed (found in the hair follicles). The epithelial cells cover the surface of the wound while fibroblasts and myofibroblasts (types of cells) contract to pull the wound edges together.
Stage 4: Maturation
Although the wound is covered by epithelial tissue, healing is still continuing. The wound will appear healed but remains vulnerable to damage.
Collagen in the new tissue is initially immature and disorganised, but gradually matures and comes to lie in a more organised way. Although the wound appears healed it may take several months, perhaps up to a year, for the tissue strength to reach an optimum level, and even then it may only be about 80 per cent of the original tissue’s strength.
Chapter 18: Care of children and young people with respiratory problems
18.1 Respiratory system
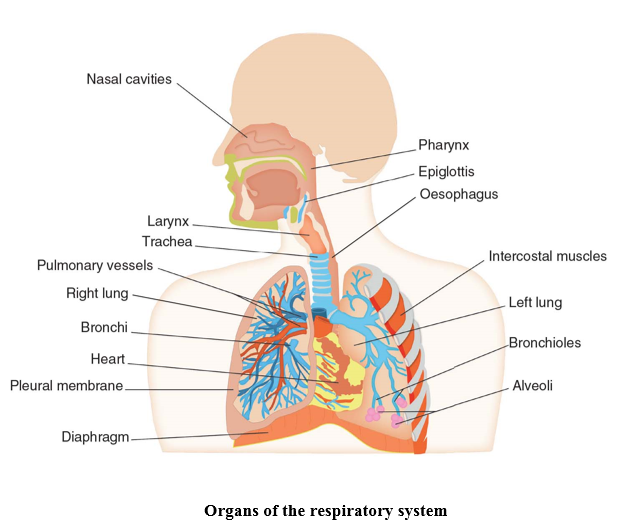
The respiratory system is divided into two main sections, the upper respiratory tract and the lower respiratory tract. The upper respiratory tract consists of the nose, pharynx and larynx, whereas the lower respiratory tract is made up of the trachea, lungs, bronchial tree and the alveoli. Although the anatomical structure of the airway is essentially the same in infants, children and adults, there are some developmental differences that must be considered.
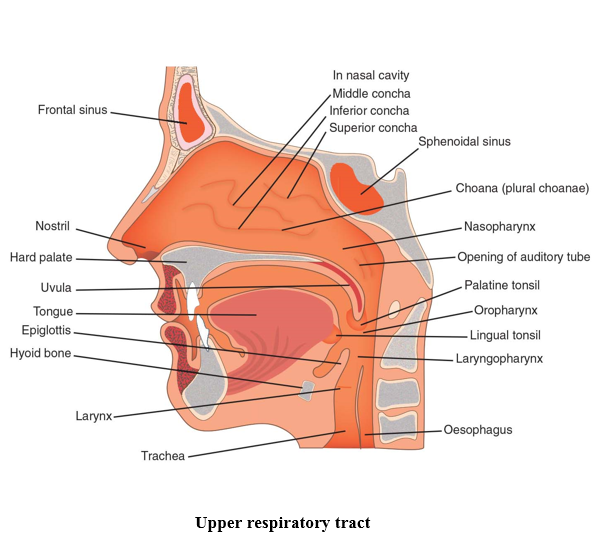
Air enters the body through the nose and passes into the nasal cavity, where shelf-like projections known as the conchae, and channels known as the meatuses, provide heat and moisture to the inhaled air before it moves further into the body. The conchae also secrete mucus and trap dust particles, which are moved by cilia towards the pharynx, where it is swallowed to avoid entering the lower respiratory tract.
The pharynx (throat) is a muscular space shared by both the respiratory and the digestive system, hence why mucus from the nose can enter the pharynx and be swallowed instead of inhaled. The pharynx is divided into three regions. The nasopharynx lies behind the nasal cavity and extends to the soft palate (rear portion of the roof of the mouth). The adenoids can be found here and act as a defence mechanism against infection. The oropharynx runs from the soft palate to the epiglottis and contains the tonsils, which like the adenoids, also act as a defence mechanism protecting the respiratory system from infection. Both food and air pass through the oropharynx. Finally, the laryngopharynx extends from the epiglottis to the oesophagus where food and fluid are conveyed to the stomach, and the larynx, which carries air to the lungs.
The larynx, also known as the voice box, is the bridge between the laryngopharynx and the trachea. The larynx is a complicated structure of cartilage, muscle and ligaments, sitting around C3-C4 in infants and children and C4-C5 in adults. The structure of the larynx produces sound as air moves over the vocal cords and also allows for movement upwards during swallowing, forcing the epiglottis down, covering the larynx and directing food towards the oesophagus. The epiglottis in the infant projects from the pharyngeal wall at a different angle to older children.
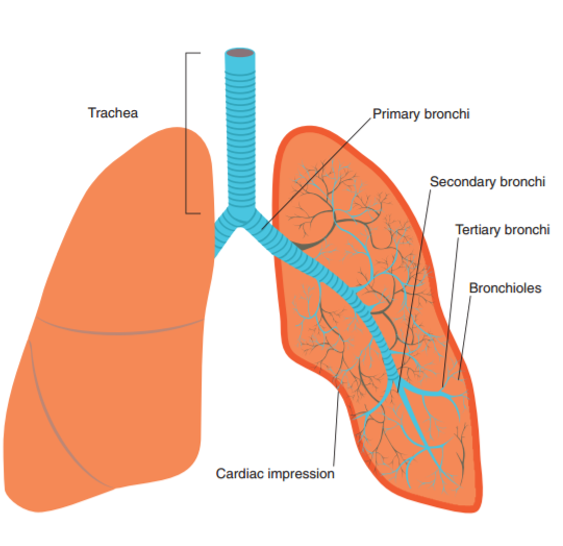
The larynx joins to the trachea (windpipe) in the lower respiratory tract, via cricoid cartilage and the cricothyroid ligament. In infants and young children, the cricoid is the narrowest part of the upper airway, whereas in the older child and adults, the narrowest point is through the vocal cord section of the larynx. The trachea is formed from C-shaped hyaline cartilage, which acts as support for the trachea. The trachea is lined with epithelial cells that produce mucus, again trapping debris and particles, which can then be expelled from the trachea through coughing, to the pharynx where it can be swallowed. The trachea in infants is narrow, soft and relatively short. As a result, even a small amount of inflammation or mucus can reduce airway size and create an increase in respiratory effort. The bottom end of the trachea divides into two smaller tubes, the right and left primary bronchi that join to the right and left lung.
The lungs are located in the thoracic cavity, extending from the diaphragm to the clavicle. The left lung is smaller than the right, to allow space for the heart. The left lung therefore has two lobes, whereas the right lung has three. Surrounding each lung is the pleural membrane. This is double layered and between the layers lies the pleural cavity. The pleural cavity contains pleural fluid, which allows for the lungs to move freely during breathing without friction against the wall of the thoracic cavity.
The bronchial tree extends from the primary bronchus to the bronchioles. The trachea divides into the two primary bronchi and these primary bronchi divide into five secondary bronchi, three in the right lung and two in the left. These secondary bronchi then divide further into eighteen tertiary bronchi; ten in the right lung and eight in the left and finally, the tertiary bronchi divide into bronchioles. The bronchioles divide further into terminal bronchioles, then respiratory bronchioles and alveoli, which is where the process of respiration takes place.
Gaseous exchange of oxygen and carbon dioxide takes place via diffusion within the alveoli, which are surrounded by capillaries. There is a continuous increase in the number and size of alveoli until approximately 8 years of age, which means the surface area available for gas exchange in infants is less than in the older child.
18.2 Respiratory embryology
The respiratory system develops relatively late in embryological terms and has no physiological function until after birth. As a result, there are implications for infants born prematurely as the final stages of lung development take place in the later stages of pregnancy.
The larynx, trachea, bronchi and lungs begin to develop during the fourth week of gestation. The lungs develop from the foregut section of the embryo, beginning first as lung buds, before separating from the foregut to create the trachea, then dividing in the fifth week into the right and left bronchi, followed by formation of the secondary bronchi. Between weeks 6–16 gestation, lung development of the bronchial tree continues and during weeks 17–26, lung development formation of the bronchioles takes place and the capillary network for gaseous exchange begins to be laid down. From week 26 onwards until birth, terminal bronchiole development takes place, alongside increased vascularisation and the appearance of elastic tissue. The formation of the capillary network and elastic tissue is required for alveoli development. True alveoli appear at around 34 weeks, with the majority of mature alveoli development taking place after birth.
Development of the nose and pharynx also begins in the fourth week of gestation. Development of the pharynx is a complex stage as folds or clefts appear in the surface of the hindbrain of the embryo to create pharyngeal pouches, giving a gill like appearance to the embryo. These pharyngeal arches, alongside the stomodeum, eventually form the structures of the face and neck. The nose is formed from the forebrain and is another complex stage of development. Nasal placodes develop from tissue in the forebrain and these develop into nasal pits. The nasal pits deepen and extend into the oral cavity, until fusion of the secondary palate occurs to separate the nose and mouth. Epithelial cells plug the nasal cavity by weeks 7–8 and continue to occlude the nasal cavity until week 17 when the plug disintegrates and the nasal passage is re-opened. During this time, the nasal conchae also develop. The structures of the upper airway continue to delineate and grow throughout the remainder of pregnancy.
Respiration by the developing foetus takes place through the mechanism of foetal circulation via the placenta. Although foetal breath movements are seen, breathing does not occur until after birth. During pregnancy, the foetal lungs are filled with foetal lung fluid and must empty at birth. The process to achieve this begins a few days before the pregnancy reaches term, when pulmonary epithelium becomes sensitive to stress hormones. When labour begins, stress hormones in the foetus rise and foetal lung liquid begins to be reabsorbed into the body. Normal vaginal delivery compresses the chest wall, increasing intrathoracic pressure, which drains the lungs further. Babies born by caesarean section may retain some foetal lung fluid, requiring monitoring in the neonatal unit.
Chapter 19: Care of children and young people with cardiovascular problems
19.1 Cardiac anatomy
Cardiac anatomy
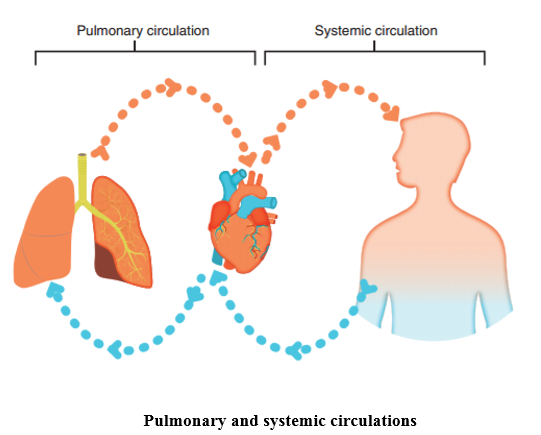
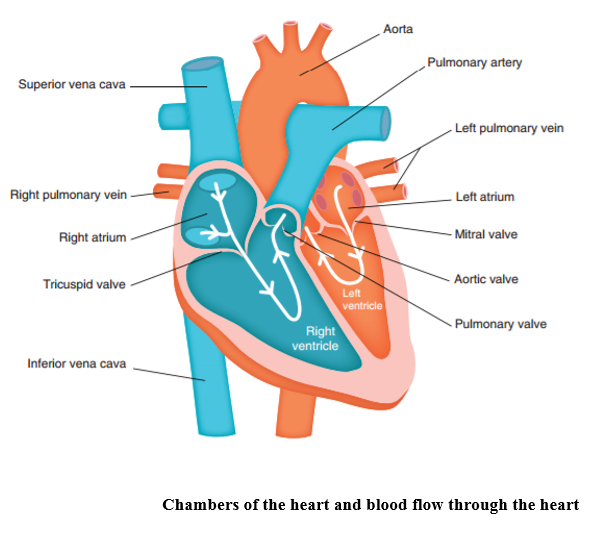
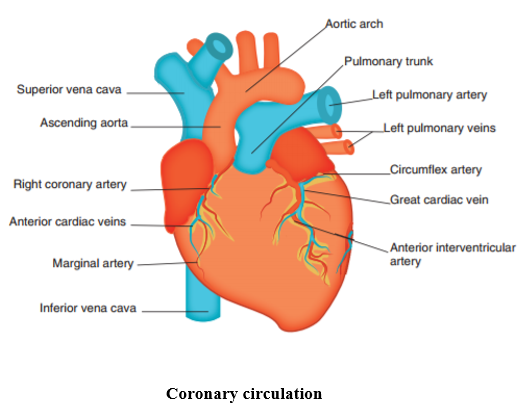
At a basic level, the heart is a pump that circulates blood around the body. It consists of two pumps, the left side and the right side, which work in a figure of eight, passing deoxygenated blood from body through the right-hand pump to the lungs and receiving oxygenated blood from the lungs, through the left side of the heart and back out to the body. Because the lungs are in close proximity to the heart, the right side of the heart has less work to perform than the left side of the heart. This is the reason why the myocardium on the left side of the heart is thicker than on the right.
The heart is composed of three layers – the pericardium, the myocardium and the endocardium. The pericardium covers the outside of the heart, protecting it from structural damage and providing lubrication to ensure the heart can move without friction against other nearby anatomical structures.
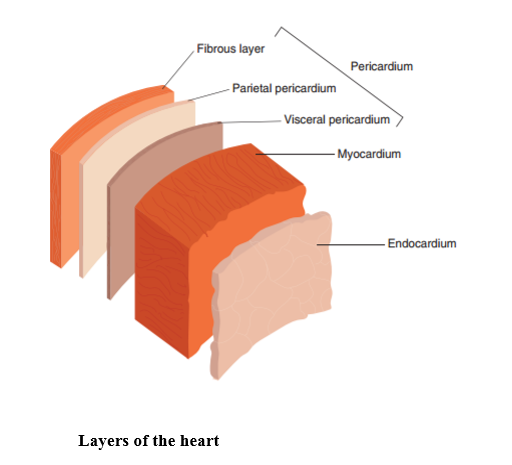
The myocardium (heart muscle) varies in thickness depending on the strength needed by each chamber. This means the atrial chambers are thinner than the ventricular chambers and the left side is thicker than the right side. The inside lining of the heart, the endocardium, consists of epithelial cells which provide a smooth surface for blood to flow over; however, parts of the right ventricle and two thirds of the septum have a rougher surface, and form part of heart’s conduction system.
Inside the heart, there are four chambers – two atria and two ventricles, one for each side. The atria receive blood and pump it to the ventricles and the ventricles then pump that blood, at force, out to its destination. The atria and ventricles are separated from each other by atrioventricular valves which ensure a one-way flow through the heart. The exit from the ventricles into the pulmonary artery and the aorta are also protected by one-way valves, the pulmonary valve and the aortic valve.
Embryology
Heart development begins around 18 days post fertilisation. Between day 20 and 21, the endocardial tubes form and fuse and between days 22 and 25, the cardiac loop forms and the chambers begin to develop. Formation of the cardiac septum takes place around day 27 and by day 28, the heart has four recognisable chambers and has begun to beat. Formation of the major vessels occurs at around day 29 and by day 56 (8 weeks gestation), the heart is fully developed, therefore congenital malformation of the heart occurs in very early pregnancy, possibly before the pregnancy is confirmed. This is important because whilst most congenital heart disease is thought to be idiopathic (no known cause), there are environmental factors which predispose the foetus to congenital heart disease. These include both prescription and illegal drugs, alcohol, rubella infection and maternal disease, such as diabetes mellitus.
In utero, the mother’s placenta provides oxygen to the foetus and the lungs are not required for oxygenation until after birth. This means that the circulation in the foetus differs, with the presence of structural anomalies (a connection between the two atria and a connection between the aorta and pulmonary artery) which allows a certain amount of blood to by-pass the lungs. After birth, these connections should spontaneously close as a result of physiological changes and the difference in pressure between the left and the right side of the heart – as the left side of the heart pressure increases to maintain circulation to the body, the pressure on the right side of the heart decreases and the movement of blood from the right atria to the left atria and the pulmonary artery to the aorta decreases, allowing for closure of the two connections. Sometimes, one or both of these connections fail to close post birth, becoming a structural defect in their own right.
19.2 Conduction system
The heart is able to pump due to its own conduction system, which enables it to initiate and conduct an electrical impulse. The conduction system consists of:
- The sinoatrial node (SA node)
- The atrioventricular node (AV node)
- The atrioventricular bundle (AV bundle) or bundle of His
- Right and left bundle branches
- Purkinje fibres
The sinoatrial node acts as the pacemaker, initiating an impulse which causes atrial contraction (atrial systole). The impulse then spreads until it reaches the atrioventricular node, from which it travels to the ventricles through the atrioventricular bundle (bundle of His) to the Purkinje fibres to cause contraction of the ventricles (ventricular systole). There is then a brief period of recovery (diastole) before the next impulse is generated.
Chapter 20: Care of children and young people with neurological problems
20.1 Nervous system
It is a good for those who work with patients with neurological problems to know a little of the structure and complexity of the nervous system. This online resource will provide an overview of the nervous system to cast some light on the underlying anatomy and physiology to enable practitioners to better understand the impact of disease.
The nervous system
The nervous system is made up of two parts. The first part is the Central Nervous System (CNS), which consists of the brain and spinal cord. The second part is the Peripheral Nervous System (PNS) which contains the nerves responsible for sending and receiving information to the CNS. The PNS includes all nerves outside of the brain and spinal cord and includes 31 pairs of spinal nerves as well as 12 cranial nerves.
The brain
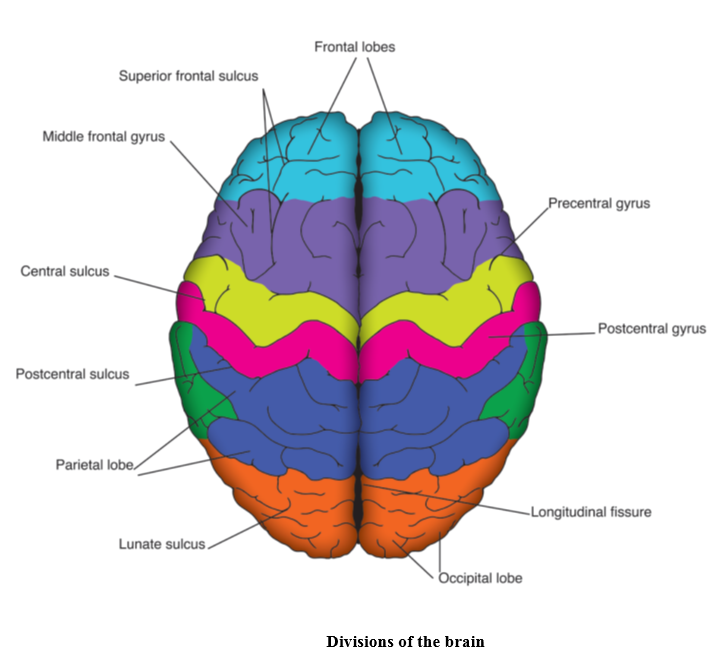
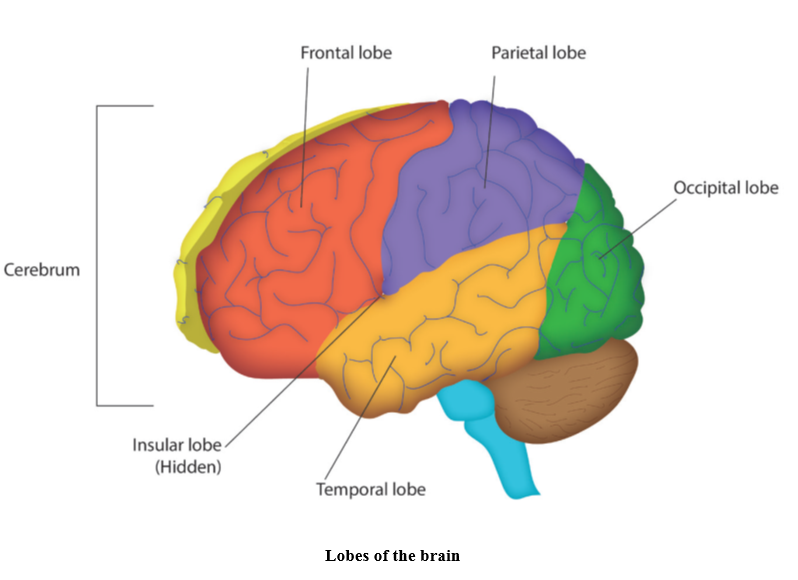
The brain has the consistency of blancmange and weighs approximately 1.5kg in adults. At birth the main brain structures are in place and major nerve tracts are functioning; however, further neurological maturation occurs throughout childhood and by 7 years the brain is almost adult size (Kagan and Herschkowitz, 2005). The largest part of the brain is the cerebrum which consists of two hemispheres, each responsible for controlling and receiving information from the opposite side of the body. The fibres going between the two hemispheres (the corpus callosum) bring together experiences associated with the activity of the hemispheres. The cerebral cortex, which covers the entire cerebrum, is divided into four specialised lobes and each performs different functions:
- The frontal lobe is crucial for complex mental functions such as judgement and emotional control as well as containing the motor areas associated with voluntary movement and language
- The temporal lobe receives information from the ears and is associated with language, understanding speech and memory formation
- The parietal lobe contains the somatosensory areas which process sensory information from the body and is associated with the integration of vision, memory and action.
- The occipital lobe is located at the back of the brain and consists of specialist areas responsible for processing visual information.
20.2 The CSF pathways
CSF circulation
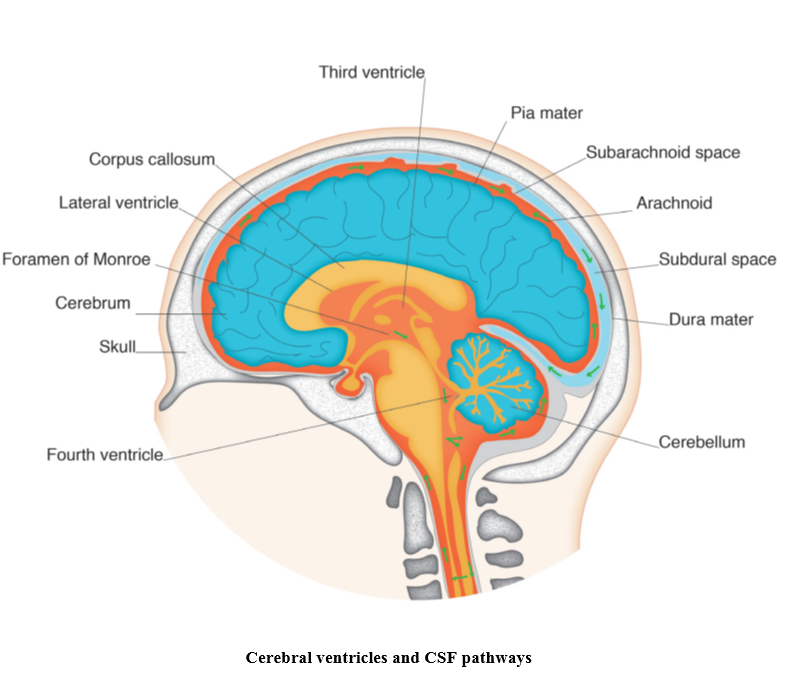
CSF circulates from the lateral ventricles into the third ventricle via the foramen of Monroe to the fourth ventricle where it passes into the arachnoid spaces. Most of the CSF passes up and around the brainstem, through the tentorial hiatus and basal cisterns and into the arachnoid space of the cerebral hemispheres and spinal cord. The bulk of CSF is absorbed via the arachnoid villi (Crossman and Neary, 2014).
References
Crossman, A. and Neary, D. (2014) Neuroanatomy: An Illustrated Colour Text. Edinburgh: Churchill Livingstone.
Kagan, J. and Herschkowitz, N. (2005) A Young Mind in a Growing Body. New Jersey: Lawrence Erlbaum Associates.
Chapter 21: Care of children and young people with urinary/renal problems
21.1 Renal anatomy
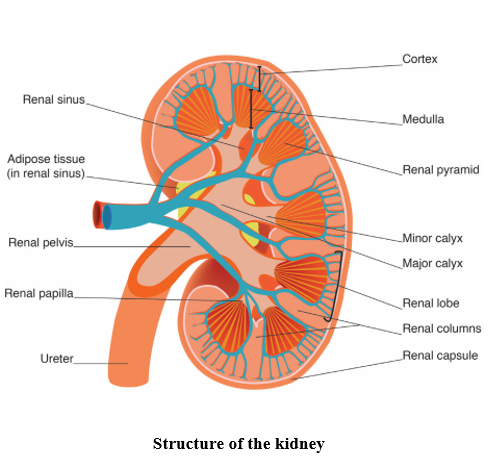
(All reproduced from Boore et al. (2016) Essentials of Anatomy and Physiology for Nursing Practice. London: SAGE, pp. 295–296.)
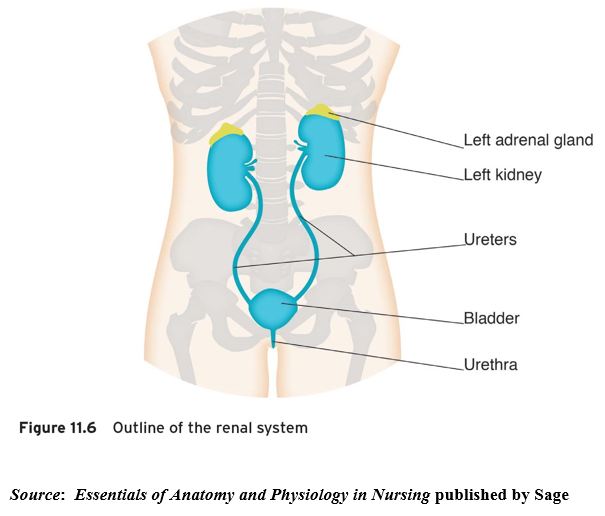
The renal system is one of the excretory systems of the body and is composed of two kidneys, two ureters (one from each kidney) which transport urine to the bladder, and one urethra enabling excretion of urine from the body. The renal system has a number of key functions: excretion (removal of organic wastes from body fluids); elimination (discharge of waste products); and homeostatic regulation.
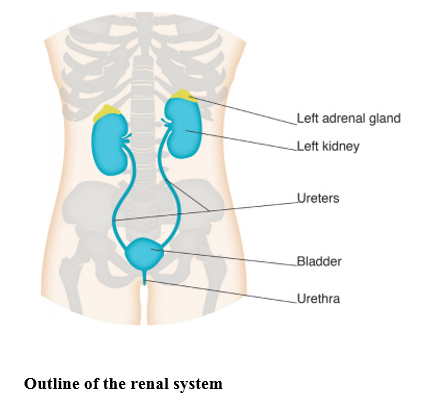
The kidneys are positioned as shown above, on the posterior wall of the abdomen within the peritoneal cavity and their structure is illustrated below. They are about 11–14 cm (4.3–5.5 inches) in length, 6 cm (2.4 inches) wide and 4 cm (1.6 inches) thick. Three layers of tissue surround each kidney: the renal capsule, the adipose capsule and the renal fascia. The renal capsule is the innermost layer and consists of a smooth, transparent sheet of irregular connective tissue that is continuous with the outer coat of the ureter: it serves as a barrier against trauma and helps maintain the shape of the kidney. The adipose capsule is the middle layer and is a mass of fatty tissue which surrounds the renal capsule, protecting the kidney from trauma and holding it firmly in place in the abdominal cavity. The renal fascia is the outermost layer consisting of a thin layer of dense irregular connective tissue that anchors the kidney to the surrounding structures and to the posterior abdominal wall. There are two distinct regions within the kidney: the renal cortex and the renal medulla. The renal cortex extends from the renal capsule to the bases of the renal pyramids and into spaces between them. The area that extends between the renal pyramids is known as the renal column. Within the renal cortex there are two zones: the cortical zone (outer) and the juxtamedullary zone (inner). The renal medulla is the innermost layer, consisting of pale conical-shaped striations known as renal pyramids (consisting of the base and renal papilla or apex). The base of the pyramid faces the renal cortex and its apex points toward the renal hilum. A renal lobe thereby consists of a renal pyramid, its overlying area of renal cortex and one half of the adjacent renal column. The nephron is the major functional unit of the kidney and filtrate formed here drains into papillary ducts (which extend through the renal papillae) and into minor (8–18) and major (2–3) calyces (cuplike structures). A minor calyx receives urine from the papillary ducts of one renal papilla and delivers it to a major calyx; once the filtrate enters the calyx it becomes known as urine as no further reabsorption can take place.
To find out more about the renal system, you can watch the following video:
Nephrology – Kidney and Nephron Overview. Available at: www.youtube.com/watch?v=Ioir82UA9x4
22.2 Thyroid
This is situated at the front of the neck and has four parathyroid glands embedded in it.
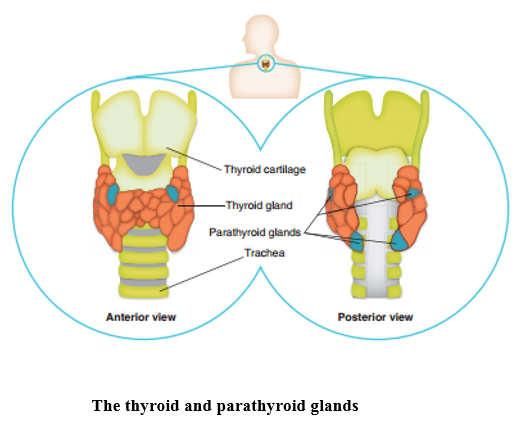
The thyroid gland produces the hormones thyroxine (T4) and triiodothyronine (T3) under the influence of TSH from the anterior pituitary gland controlled by thyrotropin releasing hormone (TRH) from the hypothalamus. Thyroid gland tissue is composed of follicles containing the colloid thyroglobulin (a gelatinous glycoprotein containing suspended particles) surrounded by the follicular cells which make it. The process of formation of the thyroid hormones starts with two parallel pathways:
- Iodine is trapped and absorbed into the follicular cells as active iodine and passed into the follicle
- Thyroglobulin is formed in the follicular cells and also passes into the follicle
In the follicle, the iodine becomes attached to the amino acid tyrosine in the thyroglobulin to form monoiodotyrosine (MIT) and diiodotyrosine (DIT). Two DITs combine to form thyroxine (T4) while one MIT with one DIT forms triiodothyronine (T3). Small amounts of the thyroglobulin are taken back into the follicular cells and digested to release T3 and T4 which are then transported into the blood stream. The thyroid hormones increase the basal metabolic rate of the body, regulate metabolism of all nutrients and are essential for normal growth and development of all body cells. They also stimulate heat generation. The parafollicular cells, also in the thyroid gland, secrete the hormone calcitonin which, with parathyroid hormone (PTH), is involved in calcium metabolism.
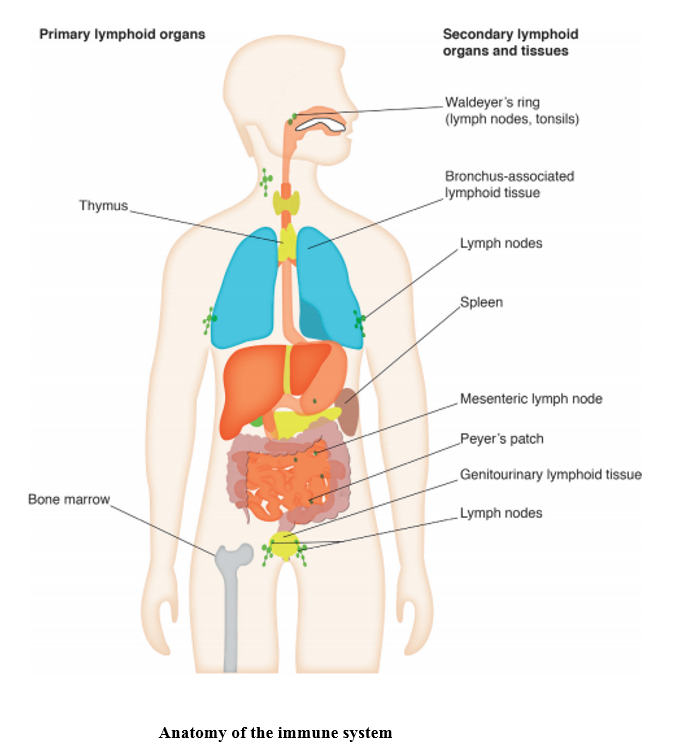
Chapter 23: Care of children and young people with immunological problems
23.1 Immune system
To find out more about the immune system, you can watch the following video:
Chapter 24: Care of children and young people with musculosketetal problems
24.1 Skeleton & muscles
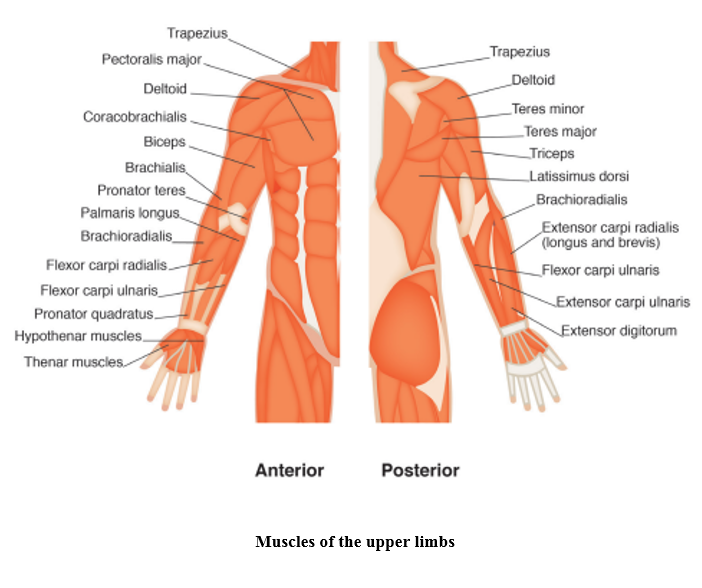
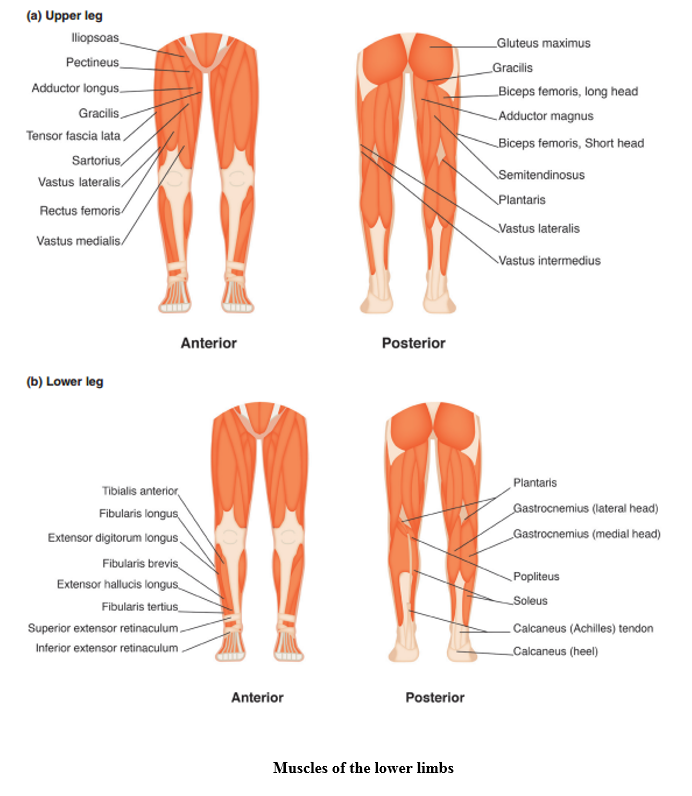
To develop your knowledge to be able to nurse the child with an orthopaedic problem, it is essential to have an understanding of skeletal and muscle anatomy and function.
The child’s skeleton is not fully formed, with parts made up of cartilage. As the child’s skeleton matures, the cartilaginous parts become bone and fuse, eventually forming the adult skeleton of 206 bones.
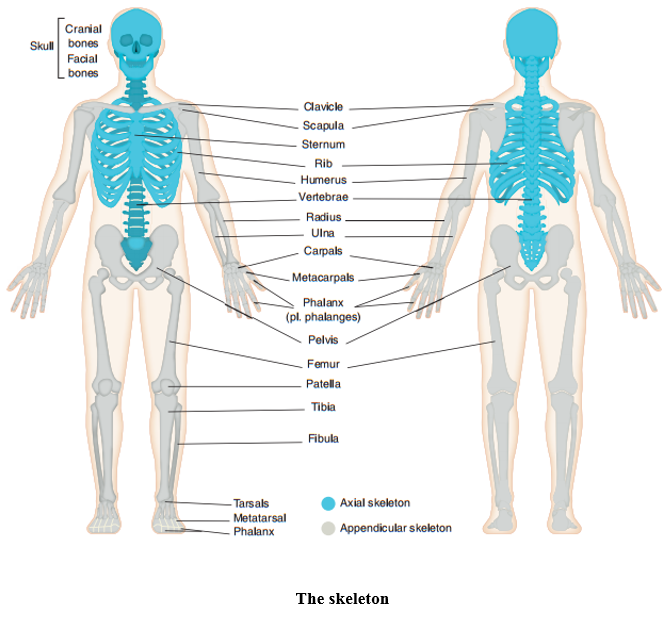
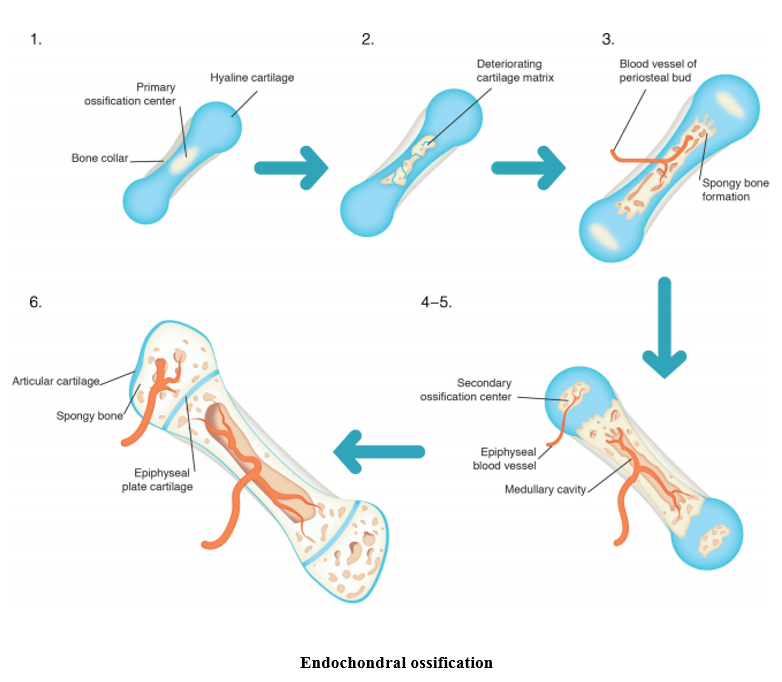
The main function of the skeleton is to protect the vital organs of the body, provide a framework for muscle attachments to allow movement, store minerals, produce red blood cells and to give the body shape.
To understand the process of bone healing after a fracture watch this video clip on bones, fractures and repair:
www.youtube.com/watch?v=MNkI6Of2PRs
Skeletal muscle
The function of our muscles is to enable body movement, maintain the body’s position, store water and to generate heat.
The following website facilitates learning through videos, articles and quizzes:
Learn Anatomy at www.kenhub.com
Chapter 25: Care of children and young people with haematological problems
25.1 Haematological system
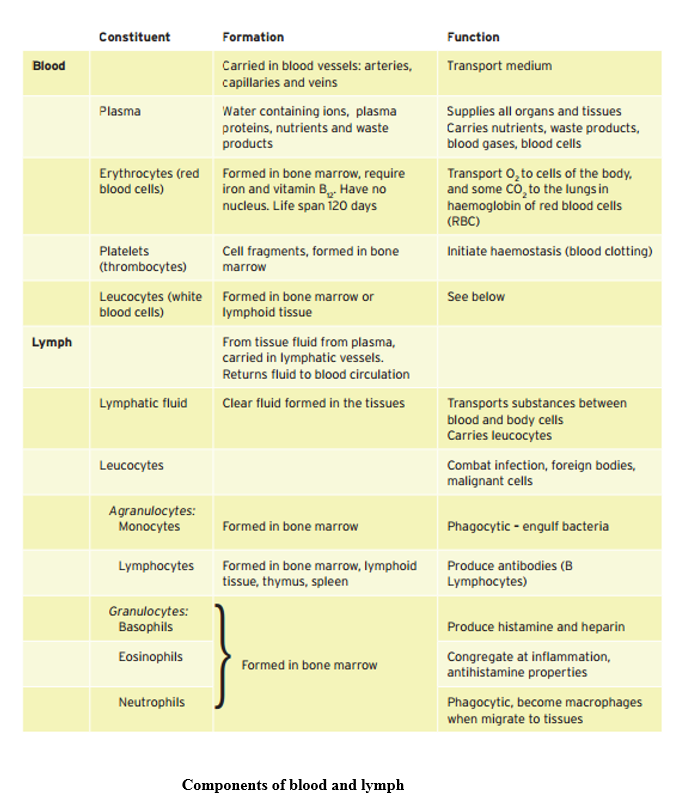
Blood and lymph
These differ from the other tissues in that the cells are not combined to form solid structures but are dispersed and transported in liquid. The table below outlines the major information about formation and functions of these tissues, which are sometimes included as connective tissues. The cells within these systems are formed from pluripotent stem cells, originally present in the embryo and capable of forming any type of body cell, which create the two multipotent stem cells from which the range of blood cells are formed.
Chapter 26: Care of children and young people with dermatological problems
26.1 Skin system
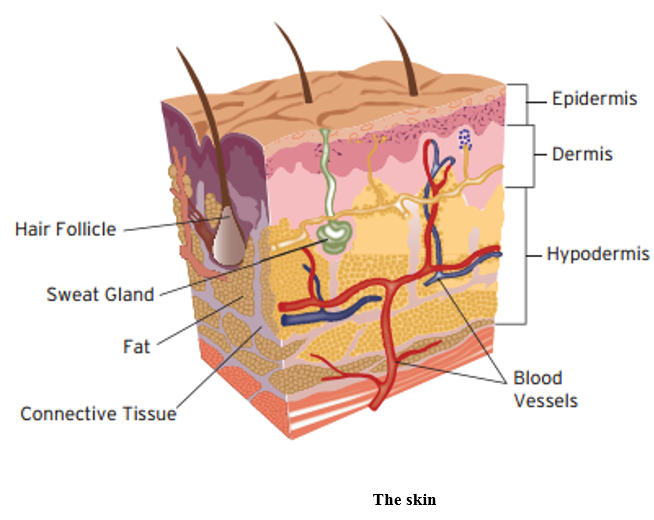
To effectively assess and care for a patient’s skin, you need to understand how it should look and what its normal functions are. The skin provides a barrier between the dry external environment and the fluid environment of bodily cells, as shown below. Skin covers the body, contains numerous sensory nerve endings, is an excretory organ, assists temperature regulation and protects the internal organs.
To find out more about the skin anatomy, you can watch the following video:
Chapter 27: Care of children and young people with thermal injury
27.1 Skin anatomy
To effectively assess and care for a patient’s skin, you need to understand how it should look and what its normal functions are. The skin provides a barrier between the dry external environment and the fluid environment of bodily cells, as shown below. Skin covers the body, contains numerous sensory nerve endings, is an excretory organ, assists temperature regulation and protects the internal organs.
To find out more about the skin anatomy, you can watch the following video:
Chapter 28: Care of children and young people with fluid and electrolyte imbalance
28.1 Renal system
The renal system consists of the kidneys (two), the ureters (one per kidney), the bladder and a urethra. The function of the renal system is to filter and discharge waste from body fluids and assist in the maintenance of homeostasis.
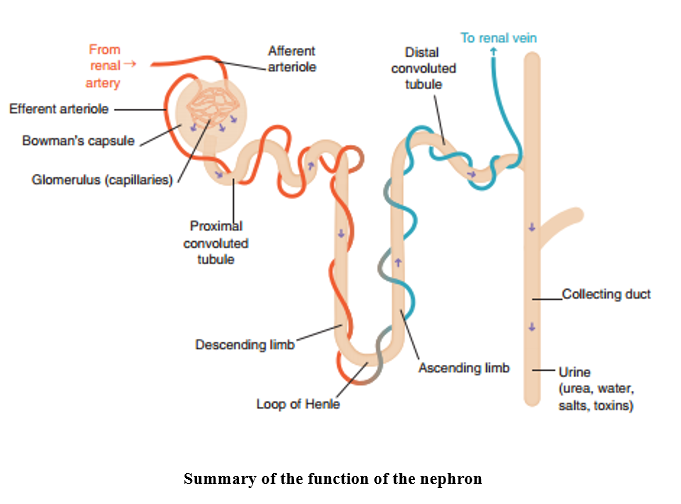
The major functional unit of the kidney is the nephron which forms urine. Blood from the renal artery enters the glomerulus in the renal corpuscle where it is filtered in the Bowman’s capsule. The filtrate contains electrolytes, urea, uric acid and creatinine and passes from the Bowman’s capsule into the proximal convoluted tubule, through the loop of Henle to the distal convoluted tubule, and finally to the collecting duct. In a healthy kidney, large amounts of nutrients and electrolytes filtered out in the Bowman’s capsule will be reabsorbed in the proximal convoluted tubule. The ascending limb of the loop of Henle is responsible for drawing sodium away from the filtrate and into the interstitial fluid via an osmotic gradient, which in turn causes water to be drawn into the interstitial fluid as the filtrate moves around the descending limb, thereby maintaining fluid concentration within the body. As the filtrate moves into the distal convoluted tubule, potassium and hydrogen ions are secreted in to the filtrate and any remaining bicarbonate is reabsorbed. Finally, the filtrate, which is now in the form of urine, reaches the collecting duct where it travels through the pelvis of the kidney and into the ureter towards the bladder.
It is through this process of filtration that blood volume and blood pressure is maintained through the adjustment of water lost in urine, electrolyte levels are controlled and blood pH is stabilised to maintain the body’s homeostatic balance.
Urine consists of approximately 95% water and 5% dissolved solids and gases. The volume and concentration of urine varies according to fluid intake and the amount of fluid lost through sweating, breathing and in faeces. The normal composition of urine includes water, urea, uric acid, creatinine, ammonia, sodium, potassium, chloride, bicarbonate, calcium, magnesium and phosphate. Urine that also contains protein, glucose, blood, ketones, white blood cells and casts may indicate infection or underlying disease.
28.2 Electrolytes
www.youtube.com/watch?v=vvGyHBWcQQU
This 10-minute video is the first in a series of videos on fluids and electrolytes, presented by a nurse lecturer. The focus is on the adult, but the principles are the same for children.
Electrolytes are either positively or negatively charged ions dissolved within body fluids and they conduct electricity when in solution. Electrolytes are obtained from the food we eat and are mainly excreted from the body via the kidneys in urine. The distribution of electrolytes within the body is not equal, for example, there is more potassium in intracellular fluid than in interstitial fluid and plasma, whereas sodium is more prevalent in interstitial fluid and plasma than in intracellular fluid.
Sodium (Na+)
Sodium is a positive ion and is a key substance in creating osmotic pressure. It plays a vital role in the conduction of nerve signals and is important in maintaining optimal functioning of the nervous system. Sodium is also important in the innervation of skeletal and cardiac muscle. The hormone, Aldosterone helps to preserve sodium levels within the body by promoting sodium reabsorption in the kidney. Excess sodium is excreted in urine.
Potassium (K+)
Potassium is also a positive ion, which is vital in controlling cellular osmotic pressure to maintain cellular hydration. Potassium plays an important role in activating cellular enzymes involved in the metabolism of carbohydrates and proteins, and is essential in the conduction of nerve signal transmission. The kidneys, either through reabsorption or excretion, control potassium levels.
Chloride (Cl-)
A negative ion, Chloride is important in the production of hydrochloric acid in the stomach, plays a role in acid-base balance and homeostasis, and assists with the transmission of nerve impulses. It is taken into the body through diet and is absorbed in the small intestine. Excess chloride is excreted by the kidneys.
Calcium (Ca2+)
The positive ion Calcium is found in heavy deposits in the bones, from where it can be released into the blood stream. Calcium is crucial in neurotransmitter release and neuromuscular excitability and it also has an important role in blood clotting. It is excreted primarily through faeces, but can also be found in urine.
Magnesium (Mg2+)
Magnesium is essential for many metabolic processes within the body and is another positive ion. It helps to keep the levels of potassium, calcium and phosphorus within intracellular fluid and is an essential electrolyte in cardiac conduction. Magnesium possesses calcium channel blocking properties within muscles, which helps to prevent arrhythmias. It is taken into the body through diet, absorbed in the small intestine and excreted by the kidneys.
Phosphate (PO43-)
Phosphate is a negative ion, which contains the mineral, phosphorus. Phosphate is important in bone mineralisation and the structural components of cells, as well as assisting in the buffering of pH, storage of adenosine triphosphate (ATP) and the transfer of oxygen. Phosphorous is obtained through diet, stored in the teeth and bones and excreted via the kidneys.
Bicarbonate (HCO3-)
Bicarbonate is a negatively charged ion and an alkaline buffer, which regulates pH within the body, helping to protect the central nervous system. Bicarbonate also plays a role in osmotic pressure and can be produced from carbonic acid (carbon dioxide dissolved in water). Homeostasis of bicarbonate is carried out in the kidney and excess is excreted in urine, but through a catalytic reaction, bicarbonate can also be converted back to carbon dioxide, which is then expelled through the lungs. Under the influence of secretin, the pancreas releases bicarbonate into the small intestine to neutralise acidic chyme as it enters the duodenum from the stomach.
Chapter 29: Care of children and young people with gastrointestinal problems
29.1 Gastrointestinal system & embryology
Gastrointestinal system
The gastrointestinal tract starts with the mouth, where food enters the body, and ends with the anus from which faecal matter is expelled. The mouth and the teeth work together to chew food (mastication), which begins the mechanical process of breaking food down for digestion. The tongue assists in the process by moving food around and to the back of the mouth for chewing and swallowing. In addition, saliva in the mouth starts the process of digestion and enables swallowing through lubrication. Infants are usually born with all 20 primary teeth present under the gums and the point at which these erupt varies. The deciduous, or ‘milk’ teeth, are replaced by permanent teeth during primary school age. This needs consideration in the child undergoing surgery as loose teeth can dislodge during intubation and become an aspiration risk.
Once food is in the oropharynx, it can be swallowed and from here, it passes into the oesophagus. Upon swallowing, the epiglottis drops down to prevent food from entering the trachea, thereby protecting the respiratory system from the inhalation of food particles. This action is not always successful and food sometimes enters the trachea, causing coughing and possible choking. Choking is a high risk for young children who have a tendency to put objects in their mouths, and is particularly common during weaning when the ability to chew food effectively is being newly established.
The oesophagus connects the stomach to the oropharynx and is a muscular tube lined with a mucus membrane. The movement of food through the oesophagus takes place via peristalsis, a wave like contraction. The cardiac sphincter at the top of the stomach allows food to enter and prevents the stomach contents from re-entering the oesophagus.
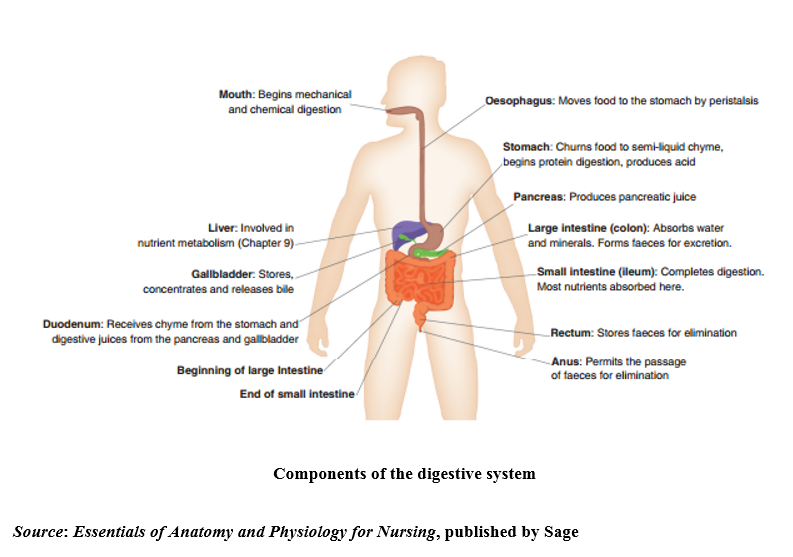
The stomach is a J-shaped sac where food is held for digestion by the closure of the pyloric sphincter at the stomach’s exit. The stomach capacity in the newborn infant is around 20mls, increasing to around 250mls by one year of age and 2500mls by adulthood. In children over the age of two years, the stomach holds a vertical position, but prior to this, it lies horizontally, which has implications for nasogastric feeding as cardiac sphincter function is compromised, increasing the risk of gastro-oesophageal reflux. Both chemical and mechanical digestion takes place here, as the stomach’s muscular construction allows for churning and mixing of the stomach contents (mechanical digestion) with gastric juices (chemical digestion) to create a substance known as chyme. The production of gastric juices is stimulated by the sight and smell of food, then once food enters the stomach, a hormone, gastrin, is produced, which further enhances gastric juice secretion. The production of gastric juices stop once the chyme passes through the pyloric sphincter and into the duodenum; chyme stimulates the release of secretin and cholecystokinin from the duodenum into the bloodstream, which in turn inhibits gastric juice production and slows stomach emptying.
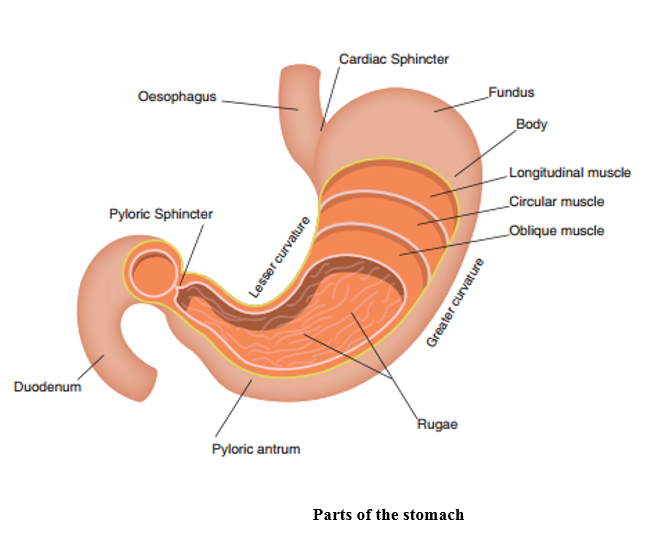
Source: Essentials of Anatomy and Physiology for Nursing, published by Sage
The speed at which the stomach empties depends on content type and volume. Carbohydrates typically digest quicker than fats, and liquids faster than solid. A recognition of this is important in nursing when preparing children and young people for general anaesthetic. Infants can usually feed closer to their theatre time than older children, however the local policy for nil by mouth times should always be followed.
The small intestine consists of three sections, the duodenum, the jejunum and the ileum and is around 275cm in length at birth, increasing to around 575cm by adulthood. Digestive enzymes from the accessory digestive organs, the pancreas and the gallbladder enter the duodenum, where the acidic gastric juices are neutralised. The pancreas releases pancreatic juices and the gallbladder stores, concentrates then releases bile that was made in the liver, to continue the digestion of carbohydrates, protein and fat in the duodenum. If bile is not released, for example, in biliary atresia, then fat is not broken down fully and cannot be absorbed, resulting in difficulty gaining weight, poor absorption of fat soluble vitamins and excess fat secretion in the faeces.
From the duodenum, chyme passes into the jejunum followed by the ileum and it is within these two structures of the small intestine where absorption of nutrients takes place. The jejunum is concerned with the absorption of nutrients and magnesium and the ileum absorbs mainly vitamin B12 and bile salts, along with any other nutrients not absorbed by the jejunum and some water. As with the oesophagus and the duodenum, chyme continues its journey through these sections of the small intestine by peristalsis. If the small intestine is unable to function correctly, then overly watery faeces will pass in to the large intestine at too high a rate for water absorption to take place, resulting in diarrhoea.
From the ileum, chyme passes through the ileocaecal valve and into the caecum. The presence of food in the stomach causes the gastroileal reflex, which opens the ileocaecal valve, allowing chyme to enter the large intestine. This in turn stimulates colonic peristalsis, the gastrocolic reflex and in time, the urge to defaecate.
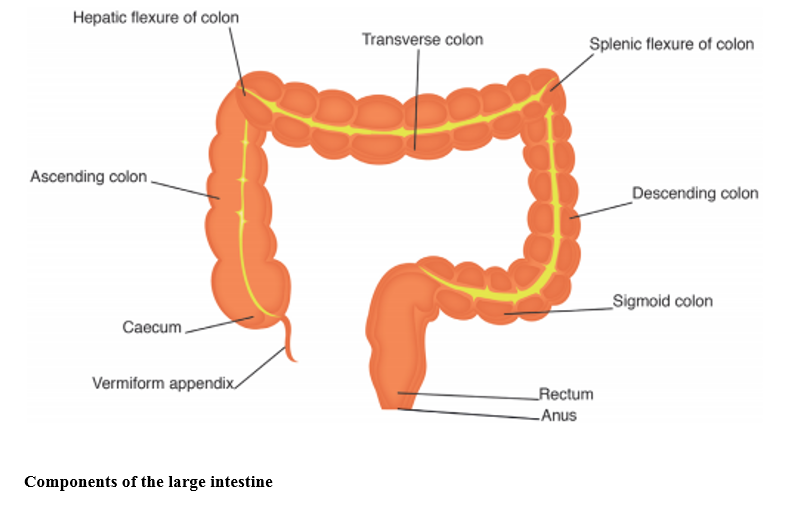
Source: Essentials of Anatomy and Physiology for Nursing, published by Sage)
The large intestine is around 40cm in length at birth, increasing to 150cm by adulthood and consists of the caecum, the colon and the rectum. Its function is to absorb water and minerals from chyme to create faeces for elimination. The caecum is attached to the appendix, a blind tube also known as the vermiform (worm-shaped) appendix. It has long been thought that the function of the appendix was lost through human evolution; however, more recent research suggests that the appendix may play a part in protecting good gut bacteria, repopulating the gut flora in the large intestine following a bout of diarrhoea. Appendicitis is thought to occur when the appendix becomes blocked, causing a build-up of bacteria which results in infection.
From the caecum, chyme then enters the ascending colon, which is situated on the right hand side of the abdomen, moving from the right to the left of the body through the transverse colon and into the descending colon on the left hand side. Chyme is moved through the colon by haustral churning. The colon is formed from a series of pouches called haustrations, which increase the overall surface area allowing for maximum water and mineral absorption. As these fill, they distend and contract, propelling the contents into the next haustration. By the time chyme reaches the large intestine, it is mainly composed of indigestible fibre, water and minerals with a large amount of bacteria. The lack of nutrients contained in chyme by this stage contributes to bacterial cell death, so that once the water is absorbed, the remaining faeces is mainly composed of dead bacteria, fibre and fermented short chain fatty acids. Adequate fluid intake is vital in creating faeces which are easy to pass and not too hard. Faeces that are depleted of water on entering the large intestine, will take longer to pass through, during which more water will be absorbed, compacting the faeces further and creating constipation.
The rectum collects and stores faeces until receptors in the rectum identify that it is full. A reflex contraction of the rectal muscles is then stimulated, the internal sphincter relaxes and faeces moves into the anal canal, which then allows for the external sphincter to be stimulated and the expulsion of faeces from the body. In young children, the urge to defaecate is involuntary, but as they grow older, children learn to recognise the sensation of a full rectum and gain voluntary control over their need to use the toilet. The physical act of defaecation, because it is voluntary, can become complicated by social and emotional aspects and may result in stool holding and a refusal to use the toilet. When the urge to defaecate is ignored, faecal content returns to the colon where more water is absorbed, potentially also contributing to constipation.
Gastrointestinal embryology
Week 3 gestation
The formation of the gastrointestinal tract begins in the third week of gestation when the primitive streak appears, the germ layers are formed (gastrulation) and the bilaminar (double layered) embryonic disc becomes trilaminar (triple layered). The primitive streak develops first and from this it is possible to determine the cranial (head) and caudal (tail) ends. The three germ layers are the ectoderm, the mesoderm and the endoderm and form the scaffold from which the various different organs and tissues will develop.
Week 4 gestation
During the fourth week of gestation, as the embryo folds and fuses, a cavity (intra-embryonic coelom) forms with a layer of endoderm and mesoderm to become the primitive gut. In this primitive gut there are three portions which can be identified; the foregut, midgut and hindgut. Initially, the midgut has a wide connection with the yolk sac, but following lateral folding of the embryo, this connecting stalk narrows to form the umbilical cord. Incomplete closure of the lateral folds causes a defect in the abdominal wall through which the intestines herniate, resulting in the congenital defect, gastroschisis. Each section of the primitive gut will eventually develop to form the gastrointestinal tract (see table below).
|
Portion of primitive gut |
Develops into |
|
Foregut |
Pharynx, lower respiratory system, oesophagus, stomach, upper section of duodenum, liver, biliary ducts, gallbladder and pancreas. |
|
Midgut |
Lower section of duodenum, jejunum, ileum, caecum, appendix, ascending colon and two-thirds of the transverse colon. |
|
Hindgut |
Remaining third of the transverse colon, descending colon, sigmoid colon, rectum, anal canal, epithelium of the bladder and most of the urethra. |
Sections of the primitive gut and associated organ development
During the fourth week, the oesophagus, stomach, duodenum, liver, gallbladder and biliary ducts all begin to develop. The position of the stomach is identifiable by a small enlargement in the foregut. Failure of the foregut to separate completely into the trachea and oesophagus during the fourth week results in trachea-oesophageal fistula and oesophageal atresia.
Weeks 5-6 gestation
During this time, there is rapid development of the organs of the gastrointestinal tract (organogenesis). As the stomach develops, unequal growth rates cause its unique curvature into the J-shape and the stomach rotates and tilts, supported by the mesentery. As the stomach develops, hypertrophy of the pylorus may result in pyloric stenosis. Neural crest cells also begin to migrate into the colon wall during this period and failure of this migration results in the presentation of Hirschprung's disease. The duodenum, which began development in week 4 undergoes epithelial cell proliferation, and the duodenal lumen becomes occluded. Massive growth of the liver begins in week 5 and in week 6, the midgut loop, which will eventually form most of the small intestine and part of the large intestine, herniates out into the umbilicus in order to allow space for it to elongate and develop. This shortage of intra-embryonic growth space is caused by the liver and kidneys which are relatively large in comparison to the surrounding organs. During week 6, the caecum and appendix first appear as a swelling on the bottom section of the midgut loop.
Weeks 7-9 gestation
In week 7, the oesophagus reaches its final length, neural crest cell migration continues and the liver continues its rapid period of growth, so that by week 9, the formation and development of blood cells in the liver has begun. The cloaca at the tail end of the embryo divides into two, the urogenital sinus and the structure that will eventually become the rectum and anal canal. By end of week 8, the anal membrane opens and becomes patent. Failure of the anal membrane to open, or the incomplete separation of the cloaca results in anorectal anomaly. Also during week 8, the gastrointestinal tract, which has undergone proliferation by the epithelial cells should experience recanalisation, the process by which the lumen of the intestine becomes open and patent. Failure of this may result in occlusion of the lumen and is another cause of oesophageal atresia or duodenal atresia. By week 8, there are also gastric pits, rugae and a layer of smooth muscle in the walls of the stomach.
Week 10 gestation
With the growth of the embryo there is an increase in the abdominal cavity space, which allows the intestines to migrate back into the cavity. As it has developed, the midgut also rotates into the correct position, with the small intestines returning and rotating first, followed by the large intestine. Failure to return to the abdominal cavity results in exomphalos (omphalocele), resulting in herniation into the umbilicus.
Once back in the abdominal cavity, the small intestine is fixed into place by the mesentery to the posterior abdominal wall, with the intestinal blood supply provided by branches of the superior mesenteric artery. Failure of midgut rotation results in malrotation, whereas failure of fixation leaves the intestinal loops at high risk of twisting and occluding the blood supply, which may lead to necrosis and ischemia of the gut. This is known as volvulus.
By the end of week 10, the liver has completed its rapid growth period and now accounts for a tenth of foetal weight. The pancreas starts to produce insulin.
Weeks 11 to term
The caecum, by week 11, is in the right iliac fossa and the developing villi are increasing the surface area of the small intestine. By week 12, the liver is producing bile and by week 13, the bile has begun to enter the duodenum and will start to move through the intestines, to give meconium its unique green colour at birth. Any defect in the biliary ducts, such as biliary atresia, will have now been established. Increasing cellular differentiation continues to enable the gastrointestinal tract to perform its unique functions. By week 16, the chief structures and parietal cells are present in the gastric pits, although the gastric mucosa does not begin to secrete hydrochloric acid until shortly before birth. The foetus can swallow amniotic fluid stimulating a limited peristalsis from week 14, but no major digestive functions happen until after birth, although the digestive enzymes are present from around 26 weeks gestation.
By 34 weeks gestation the foetus, if born, would have a sufficiently mature suck to be able to feed naturally and sucking, swallowing and peristalsis has become coordinated.
Meconium is present in the distal colon. This is formed from cellular debris, swallowed amniotic fluid and mucus from the gastrointestinal tract, and secretions from the liver and the pancreas. The anal sphincter is reactive and if the foetus encounters distress during delivery, the birth could be complicated by meconium.
During the latter stages of pregnancy all that is required is growth and maturity; however the mucosal surface of the gut will not mature fully till after birth and exposure to milk.
Source: modified from Crawford and Dixon, 2012; Chamley et al., 2005; Hill, 2017 and Moore et al., 2016
References
Chamley, C., Carson, P., Randell, D and Sandwell, M. (2005) Developmental Anatomy and Physiology of Children: A Practical Approach. London: Elsevier Churchill Livingstone.
Crawford, D. and Dixon, M. (2012) ‘Care of the infant or child with gastrointestinal or endocrine dysfunction’, in M. Dixon and D. Crawford (eds), Paediatric Intensive Care Nursing. Chichester: Wiley-Blackwell.
Hill, M.A. (2017) Embryology: Gastrointestinal Tract Development [Online]. Available at: https://embryology.med.unsw.edu.au/embryology/index.php/Gastrointestinal_Tract_Development(accessed 20 March 2017).
Moore, K.L., Persaud, T.V.N. and Torchia, M.G. (2016) Before We Are Born: Essentials of Embryology and Birth Defects, 9th edn. Philadelphia: Elsevier.
Chapter 31: Care of highly dependent and critically ill children and young people
31.1 Blood gases
Understanding blood gases is core to critical care nursing and you will learn about blood gases in your placement .This video (despite being adult-orientated) provides a simple introduction to the interpretation of blood gases to help in your placement:
www.youtube.com/watch?v=WUf-cPpnrXw
Blood gases provide information on the efficiency of oxygenation and ventilation in the lungs. Blood can be sampled from capillary, venous, central venous and arterial blood and analysed through a bedside blood gas analyser. Analysis provides information on the pH (acid-base) of the blood, partial pressures of oxygen and carbon dioxide and supports medical decision-making in the PCCU. There are normal variations between the sample type and between neonates and children. Watch this video for more understanding of blood gases: www.youtube.com/watch?v=XYUaJIBeFm4
31.2 Coagulation pathway
In order to understand what Disseminated Intravascular Coagulation is, it is important that you review what happens when injury occurs and the triggering of the coagulation pathway. The following website clearly explains using ‘chalk and talk’ in the clotting process:
Chapter 34: Care of children and young people with life limiting illness
34.1 Anecephaly
Anencephaly is a serious birth defect in which a baby is born without parts of the brain and skull, leading to foetal loss, stillbirth, or neonatal death (Obeidi et al., 2010).
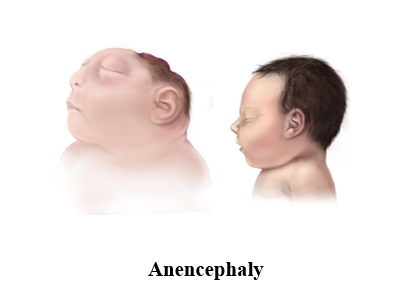
Reference
Obeidi, N., Russell, N., Higgins, J.R. and O'Donoghue, K., 2010. The natural history of anencephaly. Prenatal diagnosis, 30(4), pp.357–360.
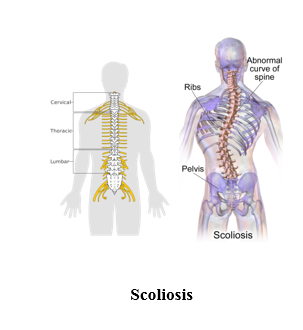
34.2 Scoliosis
Scoliosis is the abnormal twisting and curvature of the spine. It is usually first noticed by a change in appearance of the back.
Typical signs include:
- a visibly curved spine
- one shoulder being higher than the other
- one shoulder or hip being more prominent than the other
- clothes not hanging properly
- a prominent ribcage
- a difference in leg lengths
Back pain is common in adults with scoliosis. Young people with scoliosis may also experience some discomfort but it’s less likely to be severe (NHS Conditions, 2015).
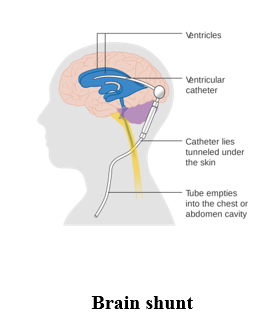
Ventriculoperitoneal shunting is a surgical intervention, this surgery is done when there is too much cerebrospinal fluid (CSF) in the brain and spinal cord, called hydrocephalus. It causes higher than normal pressure on the brain and can cause brain damage. A valve (fluid pump) is placed underneath the skin behind the ear. The valve is connected to both catheters. When extra pressure builds up around the brain, the valve opens, and excess fluid drains through the catheter into the belly or chest area, this helps lower intracranial pressure.
Chapter 36: Care of children and young people with learning disabilitiesc
36.1 Nutrition & enteral feeding
To revise the criteria for using alternative routes for nutrition in children see National Institute for Clinical Excellence at http://www.gain-ni.org/images/Uploads/Guidelines/GAIN_Guidelines_for_Caring_for_an_infant_child_or_young_person_who_requires_enteral_feeding_February_2015_Final_PDF_version.pdf
