Essentials of Anatomy and Physiology for Nursing Practice
Student Resources
Answers to Revise Questions
What is meant by the circulatory system?
Ans:
- It is the transport system of the body which carries food, oxygen, water and all other essentials to the tissue cells and which also carries away their waste products.
- It is made up of the CVS and the lymphatic system.
What are the functions of blood?
Ans: Transportation – respiratory gases, nutrients, heat, hormones and enzymes:
- To carry nutrients to the tissues
- To carry oxygen to the tissues in oxyhaemoglobin
- To carry water to the tissues
- To carry away waste products to the organs which excrete them
- To provide the materials from which glands make their secretions
- To distribute secretions of ductless glands and enzymes
- To distribute heat evenly throughout body, and so regulate body temperature
Protection – against infection, clotting, exchange of water and solutes between plasma and interstitial fluid, regulation of pH and control of body temperature.
- To fight bacterial infection through the white cells and antibodies.
- To arrest haemorrhage through clotting.
What are erythrocytes? Describe their structure and function.
Ans: Red blood cells shaped like slightly indented, flattened disks. They have no organelles and are nourished by diffusion. They contain haemoglobin, a protein–iron molecule that carries oxygen. The body contains more erythrocytes than any other type of cell, and each one has a life span of about 120 days. Erythrocytes are generated in the bone marrow through erythropoiesis.
Name the five types of white blood cells and identify their roles.
Ans:
- Granulocytes
- Neutrophils: Neutrophils engulf bacteria and cellular debris or use chemical agents to destroy them. The granules in the cytoplasm contain lysozyme and peroxidase which act as antibiotic agents. An increase in the number of neutrophils occurs in acute infections, certain malignant neoplastic diseases, and some other disorders.
- Eosinophils: These are a type of granulated leucocyte that are readily stained with eosin. Eosinophils, normally about 1–3% of the total white blood cell count, are believed to function in allergic responses and in resisting some infections. They engulf antigen–antibody complexes, allergens and inflammatory chemicals. They can also weaken or kill parasites by secreting chemical agents.
- Basophils: These are a type of granulated leucocyte that stain blue when exposed to a basic dye. Basophils normally constitute 1% or less of the total white blood cell count. They assist in the inflammatory response by secreting histamine, increasing blood flow to tissues as it is a vasodilator. They can also secrete heparin to enable leucocytes to be able to mobilise rather than being caught up in a clotting process.
- Agranulocytes
- Lymphocytes: These leucocytes contain no granules and normally make up about 25% of the total white blood cell count but increase in the presence of infection. Lymphocytes are key defence mechanisms for the body in that they can destroy cancer cells, cells that have a viral infection and cells identified as foreign. Lymphocytes occur in three forms: B-cells, T-cells and natural killer cells.
- B-cells recognise specific antigens and produce antibodies against them. Exposure to the antigen stimulates the cell to multiply rapidly, producing large numbers in the plasma.
- T-cells secrete immunologically active compounds and assist B-cells in their functions. They are cytotoxic in that they can destroy foreign cells directly. They can self-regulate other T-cells by preventing them from being overactive. They also release interleukins which stimulate other lymphocytes and macrophages (from monocytes).
- Natural killer cells provide a rapid response to virally infected cells and respond to tumour cell growth.
- Lymphocytes: These leucocytes contain no granules and normally make up about 25% of the total white blood cell count but increase in the presence of infection. Lymphocytes are key defence mechanisms for the body in that they can destroy cancer cells, cells that have a viral infection and cells identified as foreign. Lymphocytes occur in three forms: B-cells, T-cells and natural killer cells.
- Monocytes: These leucocytes are twice as large as erythrocytes and have relatively clear cytoplasm. These cells differentiate into macrophages which are large phagocytic cells. They engulf pathogens and dead neutrophils, and also clear away debris from dead or damaged cells. They also present antigens to activate other cells of the immune system.
A 40-year-old lady is admitted to hospital with acute confusion. She has a cannula in her left arm for fluid administration. In her confusion, she pulls the cannula out. What happens within her body to stop the bleeding and restore homeostasis?
Ans: Haemostasis
When a blood vessel is damaged, bleeding is stopped through a series of stages in which platelets are vital. There are three stages to this process:
- Vasoconstriction or vascular spasm: This is the immediate response in haemorrhage. Vascular spasm occurs when pain receptors mediate a fast response by stimulating the smooth muscle in blood vessels to constrict to reduce blood flow. Thrombocytes also release serotonin which causes a longer lasting vasoconstriction.
- Platelet plug formation: The inner lining (or endothelium) of blood vessels is normally very smooth and thrombocytes do not adhere to it. When a vessel is damaged, collagen fibres are exposed. Thrombocytes will adhere to collagen using pseudopods. These pseudopods will also enable them to adhere to other platelets, resulting in a mass accumulation that forms a platelet plug. These pseudopods can contract, bringing the vessel walls closer and forming a temporary seal.
- Coagulation (blood clotting): a complex series of reactions in which positive feedback enhances the process resulting in the formation of the blood clot. This process needs to be fast in the presence of a damaged blood vessel, but should not occur otherwise. Coagulation occurs by two simultaneous pathways (the intrinsic and extrinsic pathways) that then merge to a final common pathway.
Extrinsic pathway
The extrinsic pathway is activated when proteins are released by damaged blood vessels and perivascular tissue. In this process, factor III combines with factor VII. In the presence of calcium, this activates factor X.
Intrinsic pathway
The intrinsic pathway occurs from components already in the blood. It is triggered when thrombocytes release factor XII (through degranulation), leading to activated factor XI, IX and VIII in that order, each triggering the next. Factor VIII activation requires the presence of calcium and platelet factor 3 (PF3). Factor VIII will lead to factor X activation too.
Final common pathway
This stage starts with the activated factor X from both the intrinsic and extrinsic pathways. Factor X combines with factors III and V in the presence of calcium and PF3. What results is prothrombin activator. This converts factor II (prothrombin) to thrombin, which converts factor I (fibrinogen) to fibrin. Fibrin reacts with factor XIII and calcium to produce the structural framework of the blood clot. The thrombin also speeds this process up by accelerating the production of prothrombin activator by interacting with factor V.
Describe the ABO grouping system of blood.
Ans: Erythrocytes are grouped by the presence or absence of specific surface antigens on their cell membranes. These are known as A, B and O. Erythrocytes have:
- Either A or B surface antigens (Type A or Type B respectively).
- Both A and B surface antigens (Type AB).
- Neither A or B surface antigens (Type O).
Type A blood – plasma has anti-B antibodies which attack Type B surface antigens.
Type B blood – plasma has anti-A antibodies.
Type O blood – plasma has both anti-A and anti-B antibodies.
Type AB blood – plasma does not have anti-A or anti-B antibodies.
Cross reaction will occur when an antibody meets its specific surface antigen. For example, an anti-A antibody that encounters surface antigen A will cause the erythrocytes to clump/breakup. These clumps and fragments can occlude small blood vessels. Cross reactions/transfusion reactions can be prevented by ensuring that the blood type of the donor and recipient are compatible.
Describe how the cardiovascular system contributes to homeostasis.
Ans:
- It ensures every cell in the body receives all the substances needed for life – oxygen, nutrients.
- It removes waste products – carbon dioxide, ammonia, heat.
Name the components of the cardiovascular system and describe their main functions.
Ans: The key task of transport requires the CVS to have the following:
- Blood – transport medium.
- Heart – pumps the blood around the body.
- Vessels which carry the blood – arteries which carry blood away from the heart, capillaries which allow for exchange of the substances with the cells and tissues, veins which carry blood back to the heart.
- Lymphatic system – returns to the circulation any excess fluid left in the tissues.
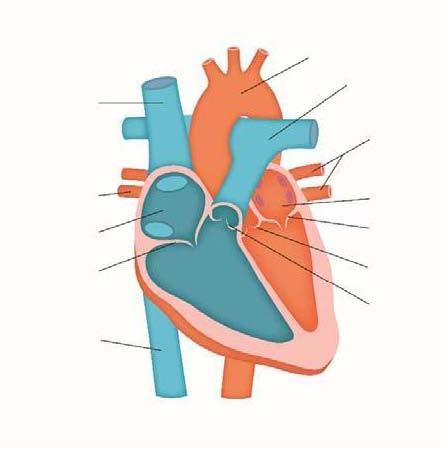
Using the diagram below to illustrate the pathway taken by the blood through the heart.
Ans:
What is blood composed of?
Ans: Blood consists of:
- 45% formed elements which are the blood cells – red, white and platelets.
- 55% plasma – a straw-coloured liquid which is a fluid connective tissue containing plasma proteins – albumin, fibrinogen, globulins.
Where are red blood cells formed?
Ans: Red bone marrow is found in the ends of the long bones, flat bones and irregular bones.
What is the stimulus for erythropoietin production?
Ans: This is controlled through negative feedback. A fall in oxygen level stimulates the release of a hormone from the kidneys called erythropoietin. This hormone increases the formation of erythrocytes. See Figure 12.1.
Describe the three layers of the heart.
Ans:
- Pericardium – outer layer made up of two sacs which cover the heart. Serous fluid between the two layers allows the heart to move easily as it contracts and relaxes.
- Myocardium – middle layer consisting of specialised muscle made up of thin filaments – actin and myosin. These allow the whole muscle to contract together ensuring the function of expelling the blood at each contraction is optimal. The myocardium is thicker in the left ventricle –think why this is so.
- Endocardium – inner layer is thin and smooth to permit smooth blood flow and reduce risk of blood clotting in the heart.
Label the diagram of the heart in question 9 to identify the components of the conduction system of the heart.
Ans: See Figure 12.17 Conduction system of the heart.
Describe how the conduction system in the heart works.
Ans: The pacemaker of the heart is the sinoatrial (SA) node, a specialised group of autorhythmic cells located in the wall of the right atrium. It is here that an electrical impulse is initiated and this impulse spreads across the rest of the atria, triggering the smooth muscle of both atria to contract at the same time. The result of this action is that blood is pumped into the ventricles. The AV node is stimulated by the impulses arriving from the SA node across the atria. Here at the AV node there is a short delay in conducting this impulse further. This allows the atria to finish contracting which gives the ventricles time to fill with blood from the atria. Once this delay is over, the nervous impulse is carried from the AV node down to the ventricles through the atrioventricular bundle (AV bundle, often referred to as the bundle of His). This specialised nerve tract divides into the right and left bundle branches and passes down the septum dividing out to each ventricle. These branches then subdivide further to cover more surface area, and these are known as the Purkinje fibres. The Purkinje fibres reach out over all of the ventricles and trigger the smooth muscle of the ventricles to contract, pumping blood out to the lungs and the rest of the body.
What are cardiac output, stroke volume and heart rate?
Ans:
- Cardiac output: The volume of blood that leaves the heart in a minute.
- Stroke volume: The volume of blood pushed out of each ventricle with each beat.
- Heart rate: The number of beats per minute.
What is blood pressure and how is it created?
Ans: The force or pressure exerted by the blood on the walls of the blood vessels. This force is created by the pumping action of the heart. The pressure in the arteries is higher than the pressure in the veins. Blood pressure is highest nearer the heart and gets lower as it moves away through the circulation. The formula for blood pressure is:
Blood Pressure = Cardiac Output × Peripheral Resistance
Describe the neural control of blood pressure.
Ans: Baroreceptors, which respond to changes in pressure, and chemoreceptors, which respond to changes in the concentration of chemicals, are found within the CVS. They measure changes in pressure and chemical substances such as carbon dioxide and oxygen in the blood. Chemoreceptors largely only respond to chemicals affected by respiration (O2, CO2 and H+). High CO2 concentration and low O2 concentrations suggest to the cardiovascular centre, located in the brain stem that gaseous exchange is suboptimal. Sympathetic stimulation will relay to the SA node to increase the heart rate (and the rate of breathing to increase gaseous exchange) to compensate. An increase in heart rate will increase cardiac output and therefore blood pressure. In contrast, if O2 concentration is high or the CO2 concentration is low then parasympathetic stimulation will relay to the SA node to slow the heart rate, dropping cardiac output and therefore blood pressure.
Baroreceptors, located in the arch of the aorta and carotid sinus, detect rises and falls in blood pressure too. A drop in blood pressure is relayed to the cardiovascular centre, which responds by sympathetic stimulation of the SA node, raising the heart rate and causing vasoconstriction of the smooth muscle in the arterial walls. Catecholamines will also be released by the adrenal medulla to raise the heart rate and to stimulate arterial vasoconstriction. Both will raise blood pressure. If the baroreceptors detect that blood pressure is too high, they relay this message to the cardiovascular centre. The cardiovascular centre then relays to the SA node, through parasympathetic stimulation, to slow the heart rate, and signals the smooth muscle in the arterial circulation to vasodilate. Both actions will drop the blood pressure.
Draw a diagram to represent the endocrine control of blood pressure.
Ans: See Figure 12.20 Renin angiotensin aldosterone system (RAAS) control of blood pressure.
