Essentials of Anatomy and Physiology for Nursing Practice
Student Resources
Answers to Revise Questions
How does an understanding of anatomy and physiology of the skin apply to nursing?
Ans: Your answer should refer to
- A number of people are vulnerable to skin integrity being compromised. An understanding of the structures and functions of the skin will enable nurses to rationalise nursing interventions to maximise skin integrity.
- The need to understand the process of wound healing – wound care is a key component of the nurse’s role.
- The need to understand the role of the skin in temperature regulation – nurses often have to care for people who are experiencing pyrexia or hypothermia, or are vulnerable to these.
- Skin is key in protecting the body from pathogens – infection control.
- Skin provides other protective factors, such as responding to pain, temperature, pressure, etc. These functions can be lost over time and make people vulnerable.
- Skin provides unique identifying details for a person – useful in forensics. Some areas of practice use fingerprints for identification of people.
- Skin is a valuable indicator of health:
- Cyanosis – indicator of inadequate oxygenation of the blood.
- Jaundice – excess of the pigment bilirubin and typically caused by obstruction of the bile duct, by liver disease, or by excessive breakdown of erythrocytes.
- Nails:
- Pale nails can indicate anaemia or circulatory disorders. Capillary refill time is also a supporting factor (should be less than 2.5 seconds).
- Inflammation of the nail fold can indicate lupus or other connective tissue disorders.
- Yellow nail syndrome is often a sign of respiratory disease, such as chronic bronchitis or lymphoedema.
- Nail clubbing is sometimes the result of hypoxaemia secondary to respiratory disease. Also associated with inflammatory bowel disease, cardiovascular disease and liver disease.
- Striations can indicate a low calcium level in the blood as well as other mineral deficiency. It also indicates protein and vitamin deficiency.
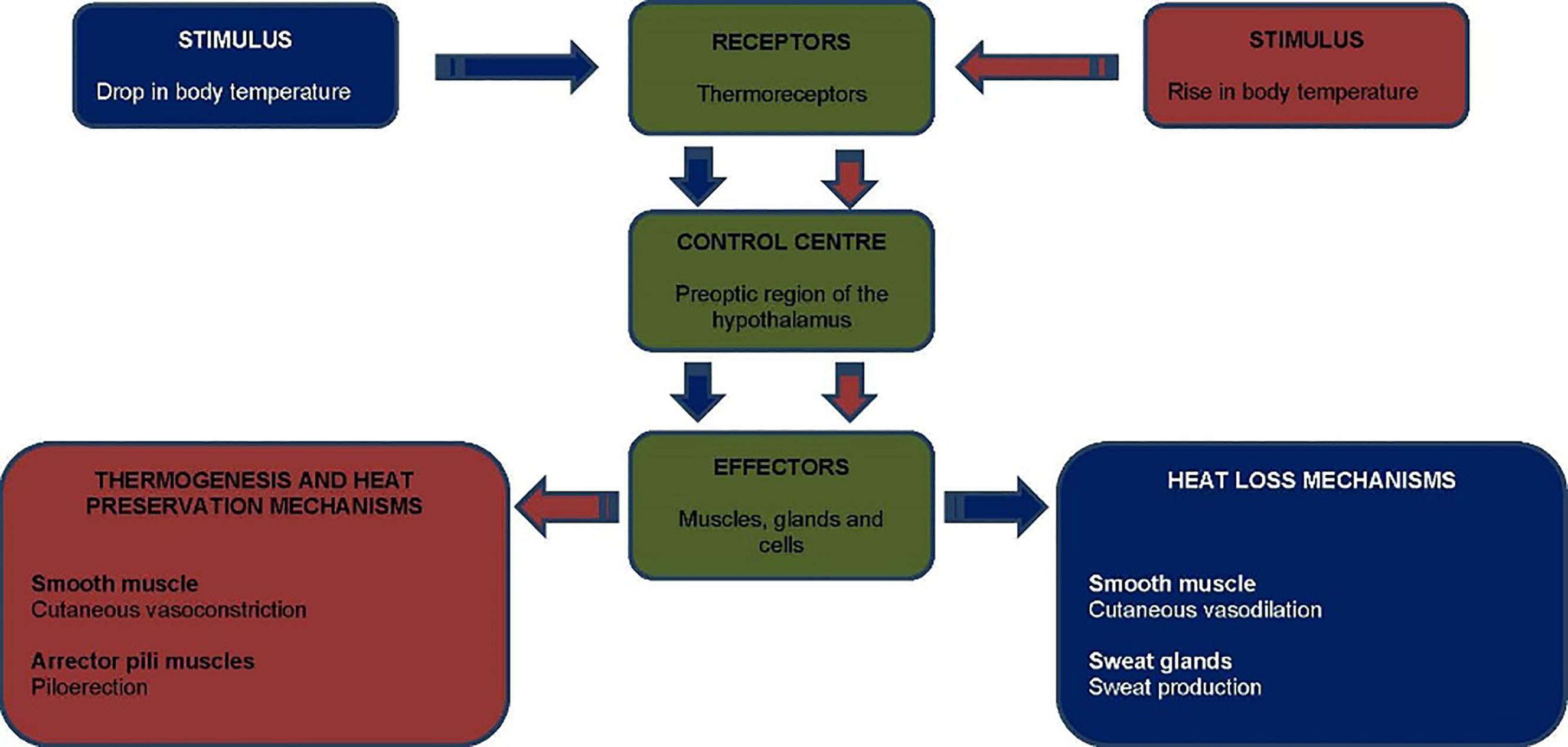
How does the body regulate temperature through the integumentary system?
Ans:
A person has a body temperature of 38.7ºC. How could a nurse help the body to achieve temperature homeostasis? You must be able to discuss the physiological responses of the nursing actions.
Ans: Nursing interventions for a person who has a fever are intended to support the body’s normal physiological processes. Nurses working with children and young people should refer to the NICE (2007) guidance on Feverish Illness in Children (http://www.nice.org.uk/Guidance/CG160) and the Royal College of Nursing’s (2007) Standards for Assessing, Measuring and Monitoring Vital Signs in Infants, Children and Young People (https://www.rcn.org.uk/-/media/royal-college-of-nursing/documents/publications/2017/may/pub-005942.pdf?la=en).
Interventions
- Administration of antipyretics (e.g. paracetamol, ibuprofen, diclofenac sodium). These are used to reduce temperature. However, antipyretic medications inhibit the inflammatory action of prostaglandins, which increase the thermoregulatory set point in the hypothalamus. Therefore, they should be used with caution – the function of the hypothalamus can be masked by antipyretics because these agents reduce the temperature and conceal the underlying signs or the cause of disease. Fever should not be treated routinely with antipyretic therapy, and the benefits and risks of using antipyretics should be assessed for individual people. It is more important to determine the cause of the fever and eliminate it.
- Cooling. External cooling measures have limitations in that they address peripheral (shell) temperature rather than core temperature. This can cause peripheral thermoreceptors to detect a decrease in temperature and tells the hypothalamus to initiate thermogenic activities such as shivering and peripheral cutaneous vasoconstriction. Tepid sponging can enhance cutaneous vasodilation if conducted correctly without telling the hypothalamus that the person is cold. However, there are few high level research studies to support its use. Cooling (as with fans and through removing bed clothes, etc.) can have an adverse effect. These interventions are largely only justified when there is neurological damage or when the hypothalamus is tricked (e.g. through keeping hands and feet warm while actively cooling the rest of the body). Shivering will increase metabolism and therefore increase body temperature. Cooling methods, as a whole, are not supported by the evidence.
- The most important intervention is to determine the cause and treat it (e.g. antibiotics, drainage of an abscess).
What are primary, secondary and tertiary healing?
Ans: Primary healing/intention
Healing by primary intention is considered uncomplicated healing. In this type of healing the wound edges are joined together and there is no tissue deficit to fill in between. There is usually no infection in the wound and scar tissue formation is minimal. The union of the wound edges occurs in a timely manner, though actual time taken to heal depends on the person’s overall health status. For example, if the person was malnourished the time taken would be much slower. In general, the initial union of wound edges takes place over 7–10 days, though the maturation stage of healing can take up to two years.
Secondary healing/intention
Healing by second intention occurs when there is a tissue deficit between the wound edges. In this situation the body must fill in and contract the wound area in order to restore tissue integrity. This involves the production of granulation tissue (delicate pink tissue) before scar tissue is formed. Wounds that heal by second intention will always have more granulation tissue in relation to size than a wound healing by first intention. The healing time is longer because of the additional need for tissue growth.
Tertiary healing/intention
Some texts will refer to tertiary intention. When a wound is intentionally kept open to allow oedema or infection to resolve or to permit removal of exudate, the wound heals by tertiary intention, or delayed primary intention. These wounds result in more scarring than wounds that heal by primary intention but less than wounds that heal by secondary intention. The mechanism of healing is similar to that of secondary intention.
What are the intrinsic and extrinsic factors that affect wound healing?
Ans: Extrinsic factors
- Mechanical stress.
- Debris.
- Temperature.
- Desiccation and maceration.
- Infection.
- Chemical stress.
- Medications.
- Other factors such as alcohol abuse, smoking and radiation therapy.
Mechanical stress
Pressure, shear and friction are all mechanical stresses and can result from immobility and/or poor positioning in bed or in a chair. They may also be localised, such as pressure from a cast or poor fitting footwear. These mechanical stresses will disrupt the circulation to the dermis, compromising the delivery of nutrients necessary for skin to live and repair. When pressure is applied to an area for sufficient time and duration, blood flow to the area is compromised and healing cannot take place. When a wound is healing, friction from the method of wound care or from contact with another surface can cause newly formed epithelium or granulation tissue to be damaged, reinitiating the inflammatory phase.
Debris
Debris, such as damaged or necrotic tissue and foreign bodies, can delay wound healing. This therefore must be removed from the site of injury during the inflammatory stage. Once this is complete, healing can progress to the proliferative stage. Necrotic tissue is removed by debridement. This can be achieved surgically or chemically.
Temperature
Temperature controls metabolism and all chemical reactions in the body. Optimal tissue repair will require metabolism to be optimal too. The external environment, nutritional status and choice of dressing will all impact on the temperature of the wound environment. Cold wounds will result in delayed healing, and too much heat will also be counterproductive as it disrupts metabolism.
Desiccation and maceration
Desiccation refers to the wound bed being too dry. Wound healing requires a moist environment. Dry wound beds are more uncomfortable, irritated and a scab (eschar) is likely to form in an attempt to retain fluid. The inflammatory and proliferative stages of healing are adversely affected by a dry wound bed.
Maceration is the opposite of desiccation, whereby the wound is excessively moist. This can be from incontinence, excess exudate or diaphoresis. Maceration can result in infection and makes the wound more susceptible to mechanical stresses. The cause must be treated, and this may include using a dressing that will manage the exudate.
Infection
Infection will prolong the inflammatory phase and delay the wound progressing to the proliferative stage of healing. Pathogens compete with the macrophages and fibroblasts for nutrition and oxygen, and this can result in their functions being inhibited and necrosis occurring. If this is extreme, sepsis and eventually death can occur. The nurse should take a swab for microbial identification from a wound suspected of being infected, and observe for the signs of infection, which include erythema (redness), heat, oedema and pain.
Chemical stress
Chemical stress is the result of cleansing products. In clinical practice, this can include the use of iodine, peroxide, chlorhexidine, alcohol and acetic acid, which with prolonged use can cause damage. They are now largely used only when there is a high risk of infection, otherwise normal saline (0.9% sodium chloride) should be used.
Medication
Certain drugs may impact on wound healing. Anti-inflammatory drugs such as steroids and non-steroidal anti-inflammatory drugs can reduce the effectiveness of the inflammatory phase. This phase is essential for removing debris and pathogens. Chemotherapy can also reduce cell division and proliferation, which is necessary for cells to divide to repair the wound. They also reduce the inflammatory response.
Other extrinsic factors
Other factors which can delay wound healing include:
- Alcohol dependency.
- Smoking.
- Radiation therapy.
Alcohol in excess can dampen the immune system. Smoking releases nicotine into the circulation and nicotine will cause vasoconstriction, which impacts on the much needed circulation and vasodilation for wound healing. Radiation suppresses the actions of leucocytes and increases the risk of infection. It can also impair cell division.
Intrinsic factors
Intrinsic factors include:
- Health status.
- Age factors.
- Body morphology.
- Nutritional status.
Health status
Chronic illness can lead to inadequate circulation, malnutrition and immunosuppression. All of these will inhibit wound healing (look back at the stages of wound healing).
Age factors
Over time, skin is damaged, thinned and less effective as an organ. This means that it is more likely to be damaged and slower to heal. Look back at the section in the chapter on age and skin.
Body morphology
Body morphology (build) has a direct impact on cutaneous circulation. Those who are malnourished and underweight may have insufficient resources for wound healing, and those who are overweight can have inadequate circulation to the area of injury.
Nutritional status
Wound healing cannot occur without the building blocks of cells and energy to permit cell division. Therefore, calories, fats, proteins, vitamins and minerals, and fluids are needed.
